Translate this page into:
Pancreatic neuroendocrine tumor trapped in a cyst
*Corresponding author: B. Archana, Department of Pathology, Sri Ramachandra Medical College, Chennai, Tamil Nadu, India. archanab@sriramachandra.edu.in
-
Received: ,
Accepted: ,
How to cite this article: Gayathri K, Archana B, Rajendiran S, Anand TK. Pancreatic neuroendocrine tumor trapped in a cyst. Sri Ramachandra J Health Sci 2021;1:28-30.
Abstract
Pancreatic neuroendocrine tumor (Pan NET) accounts for only 1–2% of pancreatic neoplasms and <1% of tumors present as cystic lesions. A diagnosis of cystic tumor in the pancreas can be very challenging and confusing. Endoscopic ultrasound (USG) and fine needle aspiration (FNA) of these cystic lesions can help the clinician to narrow down the differential diagnosis. A multidisciplinary approach is warranted for a definitive diagnosis and optimal treatment. Here, we present to you a very rare case of Pan NET presenting as a cystic mass. A 65-year-old man was admitted with a history of abdominal pain. Laboratory tests showed increased levels of serum amylase, and other biochemical tests were normal. The patient underwent transabdominal USG and computed tomography (CT). CT showed well-defined cystic lesion in the proximal body of the pancreas. Endoscopic guided FNA (EUS-FNA) using 22 gauges was done. Cytological examination demonstrated clusters and sheets of plasmacytoid cells. EUS core needle biopsy was done which showed loose clusters of cells with fine uniformly distributed chromatin that stained positively for insulinoma associated protein-1 which was suggestive of a Pan NET. The differential diagnosis of cystic lesions in the pancreas is very difficult with conventional radiology such as CT and magnetic resonance imaging. Cytology is helpful for a pre-operative diagnosis of cystic Pan NET. A diagnosis of Pan NET in a pancreatic biopsy or FNA with limited and suboptimal material is often challenging. This unusual case highlights the importance of pre-operative workup of EUS followed by FNAC in cystic pancreatic lesions.
Keywords
Pancreas
Tumor
Cyst
Cytology
Neuroendocrine
INTRODUCTION
Pancreatic neuroendocrine tumors (Pan NETs) are rare tumors that comprise about 5% of pancreatic malignancies.[1] The detection of Pan NETs is increasing largely due to the use of advanced imaging modalities such as computed tomography (CT), magnetic resonance imaging (MRI), and endoscopic imaging. The majority of Pan NETs are solid tumors. Rarely, they can undergo cystic degeneration, because of necrosis in a solid tumor.[2] Cystic tumors comprise only 1% and are extremely rare. Neoplastic cysts in the pancreas include intraductal papillary mucinous neoplasm (IPMN), mucinous cystadenoma, ductal adenocarcinoma with cystic degeneration, and cystic NET. A definitive diagnosis is challenging. A multidisciplinary approach by involving radiologists, surgeons, and pathologists is warranted to make an appropriate diagnosis in cases with unusual presentation to institute optimum treatment.[3] Herein, we describe a rare case of a cystic NET.
CASE REPORT
A 65-year-old man presented with abdominal pain for the past 6 months. On examination, per abdomen was soft, no organomegaly. He was a known case of Type 2 diabetes mellitus with increased serum amylase level (504 units/liter) (normal value 22–80 units/liter), and other laboratory tests were normal (CEA and CA19-9). Endoscopic ultrasound (USG) showed a cystic lesion in the body of the pancreas with no communication to the pancreatic duct. A subsequent abdominal contrast enhanced computed tomography depicted a well-defined cystic lesion within thick irregular enhancing internal septations in the proximal body of pancreas measuring 3.5 × 3.7 × 3.6 cm [Figure 1a and b] No evidence of calcification, hemorrhage, or solid components were noted. No evidence of communication with the pancreatic duct was seen. A differential diagnosis of pancreatic serous cystadenoma, mucinous cyst, and IPMN was thought of. Endoscopic USG guided fine needle aspiration (EUS-FNA) with 22-gauge needle, and subsequently, a biopsy was performed. The fluid was sent for cytological examination. The aspirate showed a highly cellular smear showing clusters and sheets of epithelial cells, some of them appearing plasmacytoid of cells [Figure 2a and b] Histopathological examination of the pancreatic biopsy showed loose clusters with nuclei showing fine uniform finely distributed chromatin. Immunohistochemical staining for insulinoma associated protein-1 (INSM-1) showed nuclear positivity with Ki 67 proliferative index was 1% [Figure 3a-c] This confirmed a diagnosis of grade 1 Pan NET.
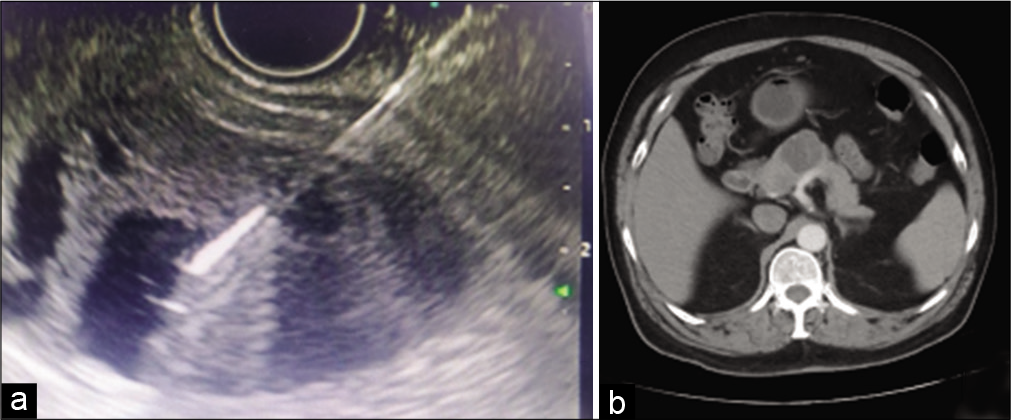
- (a) Endoscopic ultrasound showing a cystic lesion in the body of the pancreas with no communication with the pancreatic duct. (b) Abdominal contrast enhanced computed tomography showing a well-defined cystic lesion within thick irregular enhancing internal septations in the proximal body of the pancreas.

- (a and b) Endoscopic ultrasound guided fine needle aspiration showing cellular smear showing clusters and sheets of epithelial cells, some of them looking plasmacytoid with powdery chromatin.

- (a) H and E, 40×, loose clusters with nuclei showing fine uniformly distributed chromatin. (b) IHC, 40×, insulinoma associated protein-1, diffuse nuclear positive in the tumour cells. (c) IHC, 40×, Ki 67 labelling index-1%.
DISCUSSION
NETs of pancreas account for only 1–2% of all pancreatic neoplasms and <1% of all NET’s are cystic, which is very rare.[4] The mean age of diagnosis is 53 years and there is no gender predilection. Pan NETs are a rare heterogeneous group of neoplasms that arise from progenitor islet cells. PNETs may be classified as either functional or nonfunctional, depending on their ability to secrete biologically active hormones and elicit characteristic symptomatology. NETs are usually solid, and cystic NETs are extremely rare. The most cystic NETs in the pancreas are nonfunctional and the diagnosis is usually made incidentally or secondary to mass dependent symptoms such as abdominal pain and weight loss. Except for neuroendocrine microadenomas, all NETs are considered to have malignant potential and should be considered for surgical resection. Identification of cystic NETs in pancreas with imaging modalities such as CT and MRI is very difficult.[5] In the index case, a diagnosis of pancreatic serous cystadenoma was thought of. Other differentials include simple cysts, pseudocysts, and adenocarcinoma with cystic degeneration.[6] In most cases, the primary site of tumor is very small and gets noticed only after distant metastasis; thus, making the diagnosis challenging. However, it was picked up earlier in our case. CA19-9, a tumor marker is elevated in benign and malignant conditions of the pancreas such as adenocarcinomas and NET’s. Surprisingly, in the index case, it was normal, further confusing the diagnosis. EUS-FNA is an easy and cost-effective technique for the appropriate diagnosis of cystic Pan NETs. The cytomorphology of cells in a cyst fluid could be the key in the accurate diagnosis of cystic Pan NETs, just as seen in the index case.[7] The unique morphologic features of endocrine cells with coarse, stippled chromatin, and plasmacytoid cells allow for a specific diagnosis of Pan NET. Immunohistochemical staining with INSM-1[8] which is a nuclear marker of neuroendocrine differentiation has better sensitivity and specificity when compared with synaptophysin, chromogranin, and CD 56. Ki 67 proliferative index is useful for grading of these tumors and planning a definitive management. Although the management of Pan NETs has always been surgical resection, increasing frequency of the detection of small Pan NET has been challenging particularly in asymptomatic patients of advanced age who often have comorbid conditions that increase the surgical risk. In addition, nonsurgical options such as biotherapy (somatostatin analog, interferon-alpha, and bevacizumab) are useful in the treatment of grade 1 NET.[9] Interestingly, though the initial diagnosis is challenging, cystic Pan NETs have a better prognosis compared to solid Pan NETs, and these patients may be spared from extensive surgeries.[10] Thus, accurate pre-operative diagnosis is vital for patient management. The patient is currently on follow-up and the further plan of management is to take a DOTANOC scan followed by surgery.
CONCLUSION
Our case is unusual as unlike majority cases in which primary NETs are small and metastases are large, in our case, the local tumor was big. The majority Pan NETs are solid, cystic NETs are extremely rare (only 1% of NET), and CA 19-9 can also be normal in these lesions. All these highlight the unusual presentations of Pan NETs and that a high index of suspicion with a multidisciplinary team discussion is needed for an early diagnosis and instituting appropriate treatment.[11]
Acknowledgments
Nil.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Pancreatic cystic neuroendocrine tumors: Preoperative diagnosis with endoscopic ultrasound and fine-needle immunocytology. J Gastrointest Surg. 2008;12:450-6.
- [CrossRef] [PubMed] [Google Scholar]
- Cystic pancreatic neuroendocrine tumors: To date a diagnostic challenge. Int J Surg. 2015;21(Suppl 1):S44-9.
- [CrossRef] [PubMed] [Google Scholar]
- Cystic pancreatic neuroendocrine tumors: Is preoperative diagnosis possible? J Gastrointest Surg. 2002;6:66-74.
- [CrossRef] [Google Scholar]
- Cystic neuroendocrine tumor in the pancreas detected by endoscopic ultrasound and fine-needle aspiration: A case report. BMC Res Notes. 2014;7:510.
- [CrossRef] [PubMed] [Google Scholar]
- Cystic pancreatic endocrine neoplasms: A distinct tumor type? J Am Coll Surg. 2008;206:1154-8.
- [CrossRef] [PubMed] [Google Scholar]
- Cystic pancreatic neuroendocrine tumors (cPNETs): A systematic review and meta-analysis of case series. Rev Esp Enferm Dig. 2017;109:778-87.
- [CrossRef] [PubMed] [Google Scholar]
- Cystic pancreatic neuroendocrine tumors: the value of cytology in preoperative diagnosis. Cancer Cytopathol. 2014;122:435-44.
- [CrossRef] [PubMed] [Google Scholar]
- Insulinoma-associated protein 1 (INSM1) is a useful marker for pancreatic neuroendocrine tumor. Med Mol Morphol. 2018;51:32-40.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical strategy in the treatment of pancreatic neuroendocrine tumors. Jop. 2006;7:150-6.
- [Google Scholar]
- A single-center experience with pancreatic cystic neuroendocrine tumors. World J Surg Oncol. 2020;18:1-8.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic performance of endoscopic ultrasound (EUS)/endoscopic ultrasound--fine needle aspiration (EUS-FNA) cytology in solid and cystic pancreatic neuroendocrine tumours. J Gastrointestin Liver Dis. 2015;24:69-75.
- [CrossRef] [PubMed] [Google Scholar]






