Translate this page into:
Interpreting serology reports in dengue infection
*Corresponding author: Padmasani Venkat Ramanan, Department of Paediatrics, Sri Ramachandra Institute of Higher Education and Research, Chennai, Tamil Nadu, India. padmasani2001@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Bharathi U, Ramanan PV, Balan R, Rachana IV. Interpreting serology reports in dengue infection. Sri Ramachandra J Health Sci 2023;3:28-30.
Abstract
Dengue infection is diagnosed by the clinical picture and confirmed by laboratory evidence of dengue non-structural protein 1 (NS1) antigen (first 5 days) or dengue immunoglobulin M (IgM) antibody (beyond the 5th day). However, in secondary dengue infection, the IgM antibody levels do not rise much and the diagnosis may be missed if the levels if IgG antibodies are not considered. A 5-year-old child presented with fever, cough, and vomiting for 4 days. A diagnosis of respiratory infection was made and she was treated accordingly. She developed abdominal pain on day 3 of admission and ultrasound abdomen showed ascites and pleural effusion. Dengue fever with plasma leak was suspected. Since it was day 6 of illness, dengue serology was sent. The dengue IgM antibodies were low (5.4 IgM units [Positive >11 IgM units]).However, dengue immunoglobulin G (IgG) antibody level was 13.34 units and the IgG/IgM ratio was 2.4. A diagnosis of secondary dengue was made. The child improved with supportive measures and was subsequently discharged. To conclude, awareness about the phases of dengue fever and correct interpretation of serological tests is needed for diagnosis and appropriate management.
Keywords
Dengue serology
Immunoglobulin G
Immunoglobulin M
Interpretation
Diagnosis
Secondary dengue
INTRODUCTION
Dengue is a public health problem worldwide and in South India, the maximum transmission occurs during the period from September to December.[1] The diagnosis of dengue is usually made by epidemiology, clinical features, and hematological changes and confirmed by laboratory investigations. In primary dengue infection, in the first 5 days which is the viremic phase of infection, viral antigens like the non-structural protein 1 antigen (NS1 Ag)[2] can be detected in the blood and beyond 5 days, the diagnosis is made by detecting the presence of immunoglobulin M (IgM) antibodies. The serum immunoglobulin G (IgG) levels increase much later and persist for several months to years. Hence, IgG levels are not usually considered while making a diagnosis. However, in secondary dengue infection, the serum IgM levels may not begin to increase after day 5 while IgG levels begin to rise in the 1st week itself.[3] Knowledge about the serological changes that occur in the different phases of the infection is important to not miss the diagnosis of secondary dengue.
CASE DETAILS
A 5-year-old girl child, a known case of multi trigger wheeze, from Chennai, South India, presented with complaints of fever, cough, and vomiting for 4 days. On examination, there was no flushing, rashes, or edema suggestive of dengue fever and there was no other obvious focus of infection except the cough. The child was hemodynamically stable. A clinical diagnosis of acute respiratory infection was made. She was admitted in view of her vomiting and poor oral intake. Complete blood count was normal. The child was started on anti-pyretics and other supportive measures. Chest X-ray done was normal. On day 2 of admission, she became afebrile, but remained lethargic and had poor oral intake and on day 3, she complained of pain abdomen and had diffuse abdominal tenderness. Ultrasound abdomen showed gallbladder wall edema, mild ascites, and minimal pleural effusion. Dengue fever was suspected, her packed cell volume and platelet counts were repeated, blood was sent for dengue serology and chest X-ray was repeated. The antibody levels were IgM – 5.4 enzyme-linked immunosorbent assay (ELISA) units (positive >11 IgM units), IgG 13.34 IgG ELISA units, and IgG/IgM ratio was 2.4. The repeat chest X-ray revealed the right pleural effusion [Figure 1]. In view of increasing respiratory distress, she was shifted to pediatric intensive care unit, started on oxygen support and appropriate fluid management was continued. Her serial blood counts are depicted in [Table 1]. Blood and urine culture showed no growth, Scrub IgM was negative. She remained hemodynamically stable, the effusion resolved over the next 72 h, the respiratory distress settled, and she recovered completely. Repeat dengue serology sent on day 6 of admission showed antibody levels of IgM – 7.8 IgM units, IgG – 30.25 IgG units, and IgG/IgM Ratio – 3.8.
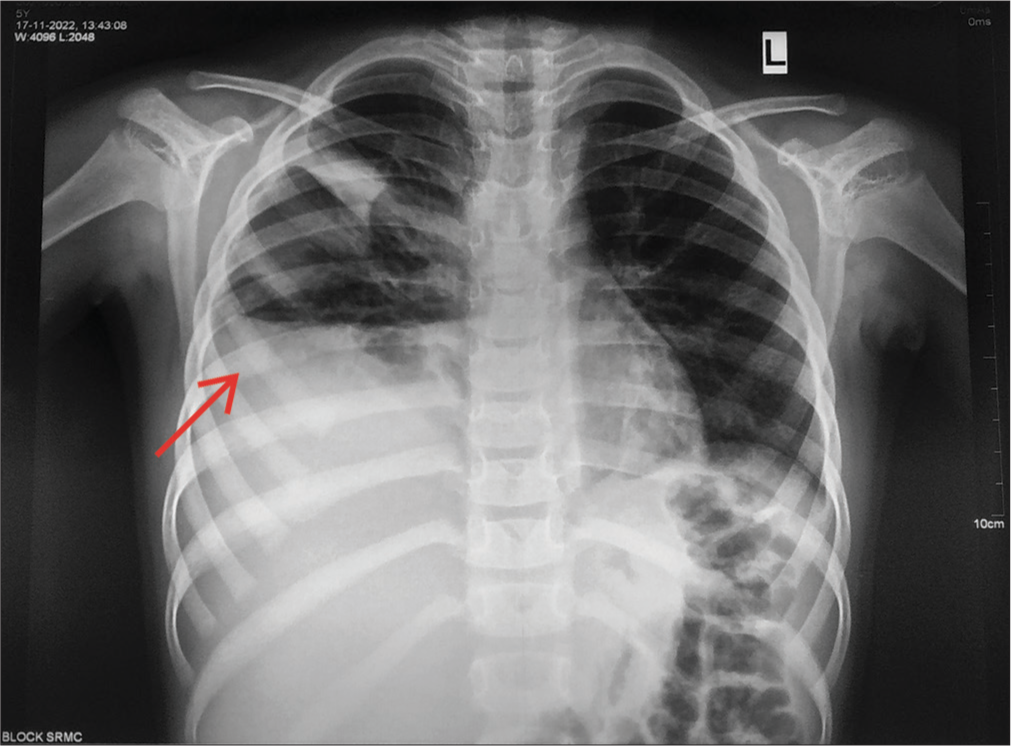
- Chest X-ray showing right sided pleural effusion on day 6 of illness (day 3 of admission).
| Day of illness | Day 4 | Day 6 | Day 7 | Day 8 | Day 9 | Day 10 | |
|---|---|---|---|---|---|---|---|
| Day of admission | Day 1 | Day 3 | Day 4 | Day 5 (6 am) | Day 5 (6 pm) | Day 6 | Day 7 |
| Hemoglobin | 11.6 | 11.2 | 11.3 | 11 | 9.7 | 10.1 | 10.6 |
| Packed cell volume | 37% | 33.6% | 33.7% | 31.8% | 28.6% | 31% | 32.9% |
| Platelets | 2.3l | 25000 | 14000 | 14000 | 39000 | 39000 | 1.42l |
| Dengue IgM (Positive >11 IgM units) | 5.4 ELISA units | 7.84 ELISA units | |||||
| Dengue IgG (Positive >11 IgG units) | 13.34 ELISA units | 30.25 ELISA units | |||||
ELISA: Enzyme-linked immunosorbent assay, IgM: Immunoglobulin M, IgG: Immunoglobulin G
DISCUSSION
Dengue fever has three phases – the febrile phase, the critical phase, and the recovery phase. During the febrile/viremic phase, the diagnosis is made by the presence of NS1 Ag. As viral load declines and fever subsides, the chances of detecting NS1 Ag falls, and diagnosis depends on correct interpretation of serology. In primary infection, IgM levels begin to rise after day 5 of illness and remain elevated for 3–8 months.[2] IgG levels begin to rise in the 2nd week and peak in the 3rd week.
In a person who has already had a dengue fever in the past, infection with another serotype of dengue virus is called secondary dengue and such infections are known to be associated with more severe illness. This is due to the more severe immunological response in the body in secondary infection.[4,5] In secondary infection, the rise in IgM levels is slower and IgG levels begin to rise earlier (by day 5).[6] This is because the presence of IgG+ memory B cells which are more likely to become antibody secreting cells while the IgM+ memory B cells are more likely to become germinal center cells.[7]
Relying only the serological tests might delay the diagnosis as in the initial few days (Day 1–3); both IgM and IgG might be negative. Furthermore, it has also been noted that more than the individual antibody levels, the IgG/IgM ratio is useful in diagnosis of secondary dengue. IgG/IgM ratio of >1.10 is considered significant.[8,9] Polymerase chain reaction remains the gold standard for identifying the infection at early stages. In a resource limited setting, dengue NS1, serology, and the ratio interpretation are more likely to help in early diagnosis.[10]
Differentiating between primary and secondary dengue is also important in clinical practice as complications are more likely to occur in secondary dengue, ranging from manifestations of plasma leak to dengue hemorrhagic fever.
CONCLUSION
Knowledge regarding the phases of presentation of dengue fever and correct interpretation of serological tests is needed for early diagnosis which, in turn, helps in timely detection of complications and their appropriate management.
Acknowledgment
We would like to thank the PICU team for their support in clinical care and the parents for permitting us to publish this case.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Dengue vector prevalence and virus infection in a rural area in south India. Trop Med Int Health. 2004;9:499-507.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of dengue NS1 test kits for the diagnosis of dengue fever. Diagn Microbiol Infect Dis. 2009;64:31-6.
- [CrossRef] [PubMed] [Google Scholar]
- Laboratory diagnosis of primary and secondary dengue infection. J Clin Virol. 2004;31:179-84.
- [CrossRef] [PubMed] [Google Scholar]
- Adaptive immune responses to primary and secondary dengue virus infections. Nat Rev Immunol. 2019;19:218-30.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of diagnostic tests: Dengue. Nat Rev Microbiol. 2010;8:S30-8.
- [CrossRef] [PubMed] [Google Scholar]
- Differentiating secondary from primary dengue using IgG to IgM ratio in early dengue: An observational hospital based clinico-serological study from North India. BMC Infect Dis. 2016;16:715.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical and laboratory predictive markers for acute dengue infection. J Biomed Sci. 2013;20:75.
- [CrossRef] [PubMed] [Google Scholar]
- Heterogeneity of memory B cells. Am J Transplant. 2018;18:779-84.
- [CrossRef] [PubMed] [Google Scholar]
- Specific IgM and IgG responses in primary and secondary dengue virus infections determined by enzyme-linked immunosorbent assay. Epidemiol Infect. 2006;134:820-5.
- [CrossRef] [PubMed] [Google Scholar]
- Dengue detection: Advances in diagnostic tools from conventional technology to point of care. Biosensors (Basel). 2021;11:206.
- [CrossRef] [PubMed] [Google Scholar]