Translate this page into:
A quality improvement intervention to improve lactation in mothers of hospitalized extreme preterm and very low birth weight infants in the first 2 weeks of life at a tertiary hospital in South India
*Corresponding author: Prakash Amboiram, Department of Neonatology, Sri Ramachandra Institute of Higher Education and Research, Chennai, Tamil Nadu, India. draprakash1@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Rajendran P, Chandran R, Balakrishnan U, Amboiram P. A quality improvement intervention to improve lactation in mothers of hospitalized extreme preterm and very low birth weight infants in the first 2 weeks of life at a tertiary hospital in South India. Sri Ramachandra J Health Sci 2021;1:16-21.
Abstract
Objectives:
Early establishment of human milk (HM) feeding significantly decreases neonatal morbidity. There are barriers in establishing and maintaining lactation in mothers of hospitalized extreme preterm and very low birth weight (VLBW) infants, particularly during the first 2 weeks of life. Infant feeding policy modification was done to improve lactation as a quality initiative project and the effect of this modification was studied.
Material and Methods:
This study was done at SRIHER by analyzing retrospective data from the period before infant feeding policy modification (April 1, 2017–June 30, 2017) and prospective data from post-policy modification (July 1, 2017–December 31, 2017). All extreme preterm babies and VLBW babies both inborn and outborn were included in the study. The policy was approved by the institutional quality control cell. Fishbone analysis and “why” question pattern were implemented to identify pitfalls in establishing and maintaining lactation in mothers of extreme preterm and VLBW mothers. Prior antenatal counseling (for inborn deliveries), immediate postnatal assessment, constant surveillance, internal audits, and regular interprofessional team meets were done to carry out the implementation of the quality control program.
Results:
Daily milk output improved after intervention from baseline value in the pre-policy modification group to nearly 3 times after policy modification. The total duration of the requirement of parenteral nutrition decreased from 11 days to 7 days and time to reach birth weight decreased from 17 days to 11 days after quality improvement initiative.
Conclusion:
A simple quality improvement initiative was able to achieve increased lactation in mothers of extreme preterm and VLBW neonates.
Keywords
Lactation
Quality improvement initiate
Very low birth weight
What is already known about the topic:
Mothers who deliver VLBW and extreme preterm infants are at risk for delayed lactogenesis and stress-mediated lactation problems which can affect milk volume adversely. Timely pumping for those mothers who are unable to put the baby to breast is an important predictor of sustained breastfeeding in the premature baby.
What this study adds:
Through quality improvement initiative using education about hand expression, proper pumping and breast milk storage techniques, continued pumping, and skin-to-skin care, the expressed breast milk volume can be increased.
INTRODUCTION
Breastfeeding is essential for infant health. However, mothers of hospitalized infants, particularly those whose babies are admitted to the neonatal intensive care unit (NICU), are unable to breastfeed effectively. The infant’s fragility, separation from the mother, and the environment present significant barriers to breastfeeding.[1] The established benefits of breast milk are vital in these medically fragile and maturational immature infants.[1] There is a dose-response relationship between the amount of human milk (HM) received by very low birth weight (VLBW) (birth weight <1500 g) infants and protection from prematurity-specific morbidities.[2] Despite the medical complexities of the NICU and shift of care to health-care professionals, mothers need to be supported for breastfeeding.[3] Health-care professional support is predictive of successful breastfeeding.[4]
There are some barriers to giving as much HM as possible to neonates during NICU stay. The majority of mothers of VLBW and extremely low birth weight infants are pump dependent and do not provide an adequate volume of milk to establish exclusive HM feedings. The application of human milk (HM) research principles and technologies in the NICU can help overcome these barriers and help us to establish adequate HM feedings in such infants.[2] Therefore, a quality improvement initiative was done to improve lactation in mothers of hospitalized extreme preterm and VLBW infants in the first 2 weeks of life. The initiative centered on health-care professional behavior change through education, modification of the individualized care plan with a breastfeeding protocol, and administration of educational materials for mothers of hospitalized infants. Mothers were educated by lactation counselors and doctors by issuing pamphlets, showing video on breastfeeding, technique of expressing milk through hand, and breast pump and peer group interaction. They were also educated on the benefits of breastfeeding, the barriers to breastfeeding, and use of breast pumps.
Specific aims
We aim to increase daily HM output in mothers of extreme preterm and VLBW neonates in SRIHER hospital from current performance to the desired level of more than 3 times of current performance by 6 months (July 1, 2017–December 31, 2017) through a modification of the existing breastfeeding policy by the implementation of the quality control program.
Secondary objectives
The secondary objectives were to compare the total duration of parenteral nutrition and the time taken to regain birth weight among extreme preterm and VLBW neonates among the groups before and after introduction of modified infant feeding policy.
MATERIALS AND METHODS
This study was done at SRIHER by analyzing the retrospective data from the period before infant feeding policy modification (April 1, 2017–June 30, 2017) and prospective data after policy modification (July 1, 2017–December 31, 2017). We obtained policy approval from the institutional quality control cell.
Study population
Inclusion criteria
All extreme preterm babies and VLBW babies both inborn and outborn were included in the study.
Exclusion criteria
Babies with surgical conditions, major congenital anomalies, and babies who died within 14 days of life and who were transferred within 14 days of life were excluded from the study. Informed consent was obtained from parents of all eligible babies. There is an existing lactation support program of the hospital. Baseline data regarding breastfeeding practices were collected from April 1, 2017, to June 30, 2017, and the mother-infant dyad was taken as the pre-policy modification group. After implementing the quality initiatives (QIs) on top of the existing lactation support program, data were collected from July 1, 2017, to December 31, 2017, and the mother-infant dyad during this period was taken as the post-policy modification group.
Specifics of the team involved in the work
A team was formed comprising neonatologists and lactation nurse. Routine care as per hospital policy for extreme preterm or VLBW infant was done by a neonatal nurse on basis of shift on duty, neonatologist on duty and assistance was provided by in-charge nurse. A separate lactation nurse assisted in establishing lactation. Initial counseling about baby care was given to attenders by the neonatologist on duty. There is no routine milk fortification policy.
Mothers of extreme preterm or VLBW neonates were accommodated in an annex building. The team identified the delay in the establishment of full feeds in extreme preterm and VLBW infants. Prioritization was done to study causes of delay in the establishment of full feeds in extreme preterm and VLBW infants. We decided to look at the data in the hospital register and neonatal case sheets to identify some problems that can be fixed. The SRIHER hospital birth register and neonatal case sheets have information about both processes of care and outcomes. Information on care at birth was collected from the records.
We used the why questioning technique to get into the depth of the problem – Why there is a delay in the establishment of full feeds in extreme preterm or VLBW infants?
The Why strategy is a simple, effective tool for uncovering the root cause of a problem. Its primary goal is to find the exact reason that causes a given problem by asking a sequence of “Why” questions. It helps in troubleshooting, problem-solving, and quality improvement initiatives. In our study, we used the why strategy to find the root cause for delay in establishment of full feeds in extreme preterm and VLBW babies.
We observed that the delay in establishment of full feeds was because mothers were unable to provide sufficient milk. The reason for not able to provide sufficient milk was that mothers were not expressing milk from day of delivery. They did not express from day of delivery as they were unaware of such practice. The mothers were unaware as there was no policy of expressing milk from day of delivery.
From Figure 1, we identified that there is a lack of practice of expressing breast milk from the day of delivery as there is no such mention in the existing infant feeding policy.
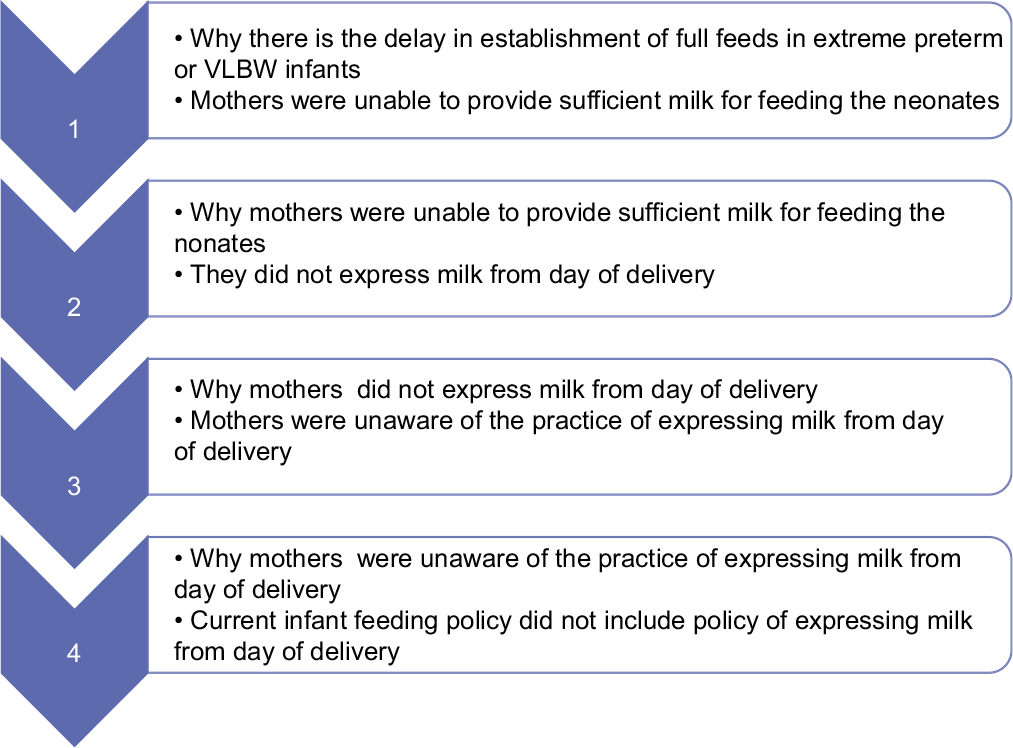
- Why questioning pattern.
A fishbone analysis, also called an Ishikawa diagram, is a visual method for root cause analysis that organizes cause-and-effect relationships into categories. It can identify many possible causes for an effect or problem. It helps in categorizing the potential causes of a problem. In our study, we used the fishbone analysis to find the various causes for mothers not expressing milk from day of delivery.
The various factors included policy, people, procedure, and place. There was no written policy of expressing milk from day of delivery. Health-care professional was unaware of benefits of early milk expression. Mothers lacked training in appropriate use of breast pump. There was no display regarding significance of breastfeeding and early milk expression in the wards. From Figure 2, barriers for mothers not able to express milk from day of delivery were identified. To overcome the above barriers, the following QI measures were undertaken:
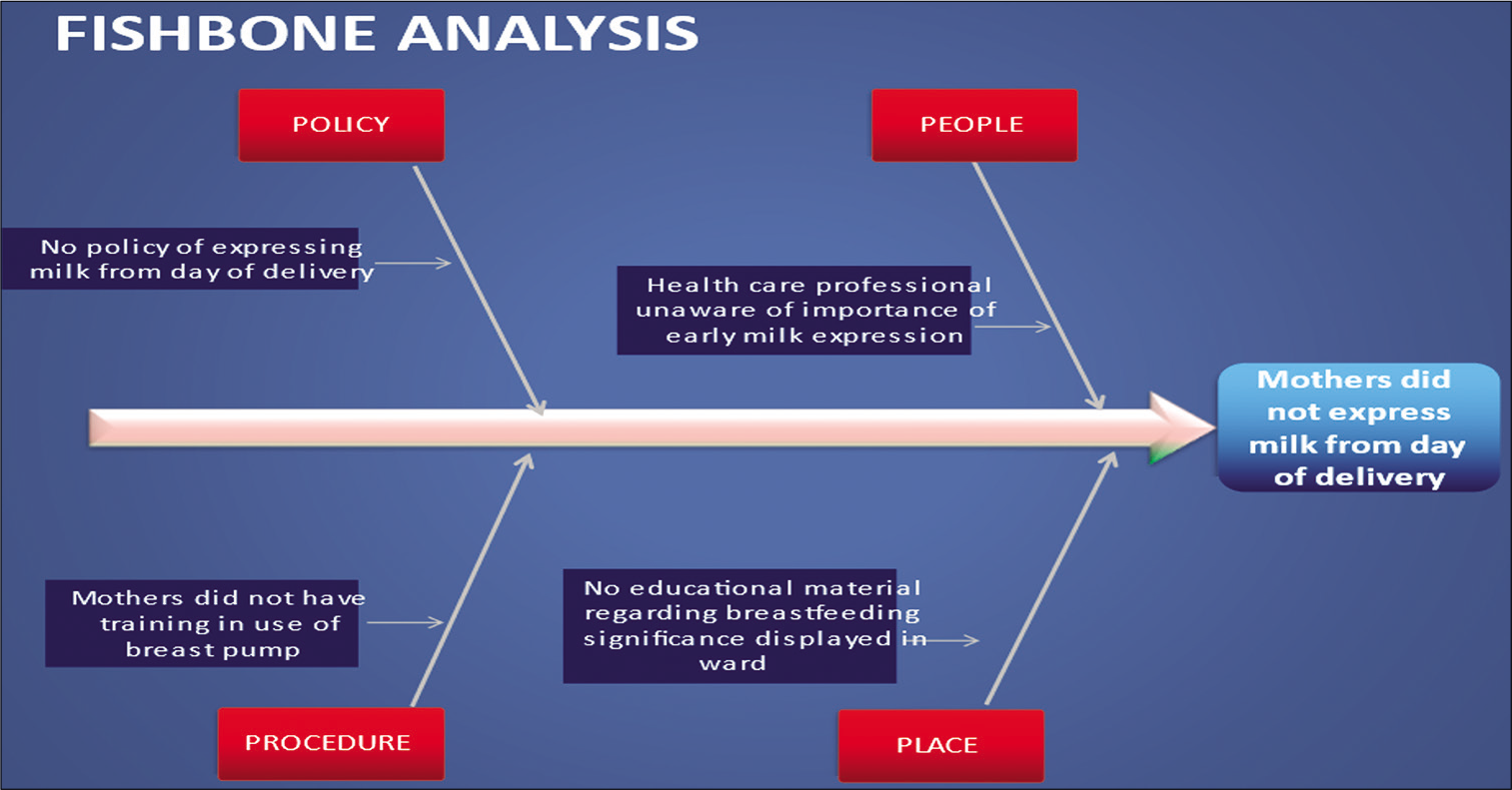
- Fishbone analysis.
Plan-do-study-act (PDSA) cycle 1
The change idea was to express milk by breast pump at regular 3 hourly intervals from the day of delivery. The team studied whether this change idea would enable the mothers to establish and maintain a milk supply. As lactation improved, this cycle was accepted.
PDSA cycle 2
The change idea was to initiate professional health education encompassing key areas of breastfeeding to mothers of extreme preterm and VLBW babies to provide adequate milk. Team studied whether this change idea would enable the mothers to improve the technique of expressing milk through hand and breast pumps. As lactation improved, this cycle was accepted.
PDSA cycle 3
The change idea was to establish breastfeeding guidelines for timely pumping, skin-to-skin contact, expressing milk since day 1 of delivery, and breast milk storage techniques. The team studied whether this change idea would enable the mothers to express more milk. As lactation improved, this cycle was accepted.
PDSA cycle 4
The change idea was to maintain a breast pump dairy to document daily milk output and counseling given every day. The team studied whether this change idea of having a breast pump diary would enable the mothers to express more milk 3 hourly even during the night. As lactation improved, this cycle was accepted.
Study design
It was a quality improvement study.
Study area
The study was done in the NICU of Sri Ramachandra Medical College and Research Institute and Sri Ramachandra Medical Centre, Chennai.
Sample size
It was a period sample. Thirty babies were studied in the pre-policy modification group and 43 babies were included in the post-policy modification group.
Data collection
Participants were recruited using a database containing all NICU admissions and discharges during the study period. Dependent variables and demographic details were collected and recorded in the pro forma.
Data analysis
Data entry and quantitative analysis were done using the Statistical Package for the Social Sciences 16 version software.
RESULTS
As mentioned in Table 1, there were 20 mothers (66.66%) in the pre-policy modification group which were primigravida and 10 were multigravida (33.33%). In the post-policy modification group, there were 35 primigravida mothers (81.39%) and 8 were multigravida (18.6%). Thirty babies were studied in the pre-policy modification group and 43 babies were included in the post-policy modification group. There were 22 male babies (73.33%) and 8 female babies (26.66%) in the pre-policy modification group. In the post-policy modification group, there were 27 male babies (62.79%) and 16 female babies (37.2%).
| Pre-policy modification group | Post-policy modification group | Chi-squared | P-value | |
|---|---|---|---|---|
| Primigravida mother | 20 (66.66%) | 35 (81.39%) | 2.035 | 0.1537 |
| Multigravida mother | 10 (33.33%) | 8 (18.6%) | 2.036 | 0.1536 |
| Male babies | 22 (73.33%) | 27 (62.79%) | 0.877 | 0.3489 |
| Female babies | 8 (26.66%) | 16 (37.2%) | 0.878 | 0.3489 |
| Outborn | 12 (40%) | 15 (34.88%) | 0.196 | 0.6579 |
| t | P-value | |||
| Mean (SD) birth weight | 1202 g (405.27) | 1135 g (1135.11) | –0.309 | 0.7580 |
| Mean (SD) gestational age | 30 weeks (2.56) | 29 weeks (29.11) | –0.187 | 0.8520 |
SD: Standard deviation
In the pre-quality improvement initiative period which was considered as the pre-policy modification group, the mean birth weight was 1.202 kg and the mean gestational age was 30 weeks. In the post-policy modification group, the mean birth weight was 1.135 kg and the mean gestational age was 29 weeks.
From Table 1, we observed that there was no statistical significant difference between the pre-policy modification group and post-policy modification group. The groups were comparable. We know that milk production varies between primi- and multi-gravida mothers. Since there was no significant difference in total number of primi- and multi-gravida mother between the two groups, the two groups were comparable.
As depicted in Figure 3, daily milk output improved from around 71 ml on day 14 in the pre-policy modification group to nearly 3 times around 285 ml on day 14 after policy modification. We observed in our study that the total duration of the requirement of PN decreased from 11 days to 7 days after infant feeding quality improvement initiative. Similarly, the time to reach birth weight decreased from 17 days to 11 days.
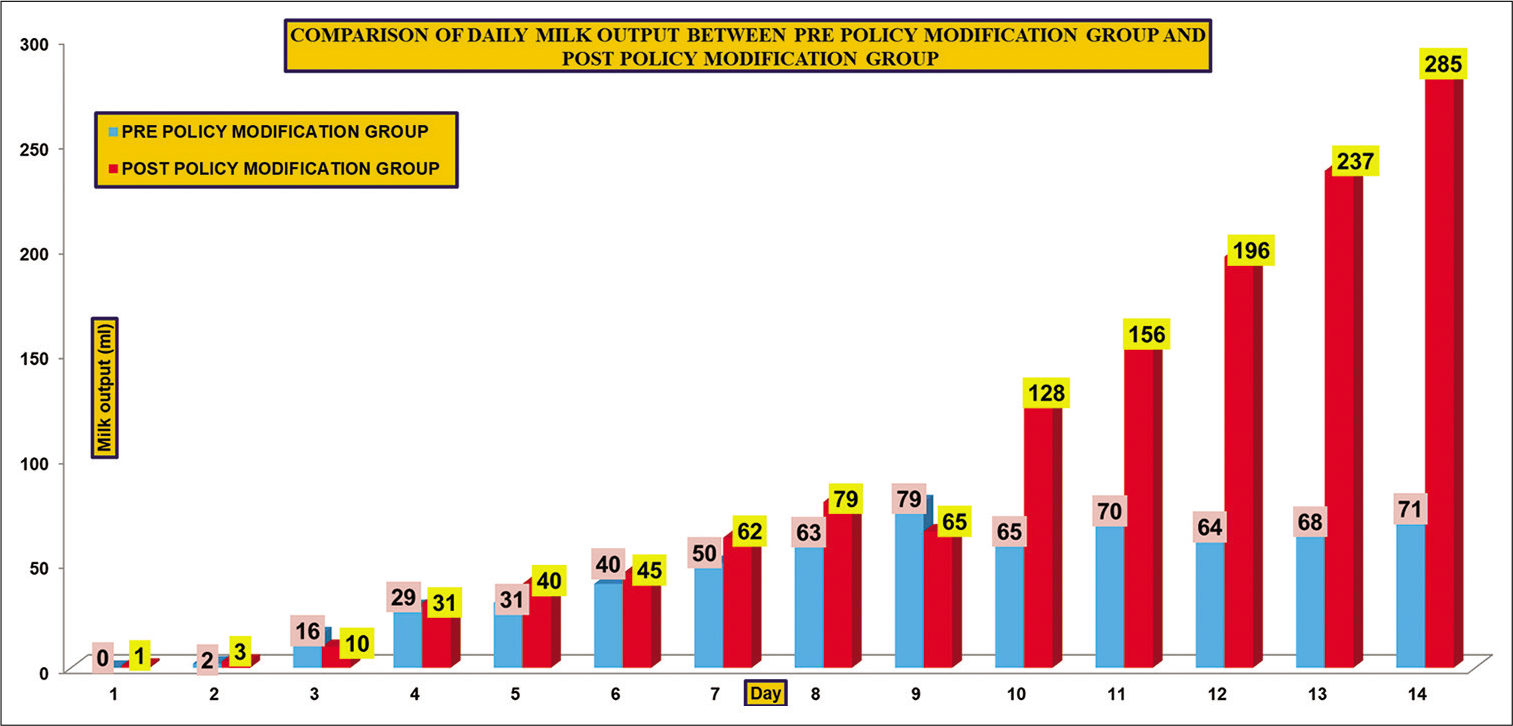
- Comparison of daily milk output between pre-policy modification group and post-policy modification group.
The mean difference in maternal milk volume was calculated on days 1, 7, and 14 in the pre- and post-policy modification groups. Between day 7 and day 1, the difference was 91.03 ml in the pre-policy modification group as compared to 63.32 ml after policy modification. Between day 14 and day 1, the difference was 130.03 ml before policy modification group as compared to 136.44 ml after policy modification. However, between day 14 and day 7, the difference was 44.8 ml in the pre-policy modification group as compared to 78.25 ml after policy modification.
DISCUSSION
The benefits of HM feeding have been observed in VLBW infants fed with their own mother’s milk and in preterm infants fed with donor HM.[5] Schanler et al. demonstrated that as compared to preterm infants who received partial HM feeds, those on exclusive HM feeds had significantly lower late-onset sepsis and necrotizing enterocolitis and a shorter duration of hospital stay.[6] However, mothers who deliver VLBW and extreme preterm infants are at risk for delayed lactogenesis and stress-mediated lactation problems which can affect milk volume adversely.[7] In our study also, we noted decrease in milk production among mothers of preterm and VLBW babies.
One barrier to breastfeeding the premature infant is that when an infant is born prematurely and warrants admission into the NICU, the mother is separated from her baby.[8] Just as the first feeding by breast is a good predictor of sustained breastfeeding in full-term infants, timely pumping for those mothers who are unable to put the baby to breast is an important predictor of sustained breastfeeding in the premature baby.[9] In our study, we observed increase in the lactation among mothers after education regarding breast pumping.
A primary reason that mothers of VLBW and extreme preterm infants have low milk volume is lack of information and equipment during the first 2 weeks after birth. Providing numerical milk volume targets and emphasizing the necessity of frequent milk expression with a hospital-grade electric breast pump will make mothers anxious.[10] The mother of a VLBW or extreme preterm neonate is sometimes pump dependent as manual expression of milk may be insufficient sometimes. In such cases, milk volume is determined completely by the effectiveness and frequency of breast pump use. Hence, NICU staff must educate mothers about the principles of lactogenesis for pump-dependent women with the use of maternal milk volume diaries or records.[11]
NICU medical staff can promote HM feeding through antenatal lactation counseling, playing music when pumping, frequent education and lactation instruction.[5] Mothers of premature infants face multiple challenges in establishing and maintaining an adequate supply of milk due to delayed secretory activation, insufficient milk volume, and difficulties in milk expression due to stress or inadequate support.[12] Pietschnig et al. observed that breastfeeding rate increased from 21.5% to 62.5% after professional support from lactation consultants.[13] We also noted a significant increase in lactation after intervention including education about breastfeeding in our study.
Meier et al. demonstrated that providing an electric pump and lactation support eliminated the differences in lactation initiation and duration.[14] We also noted that through quality control initiative using education about hand expression, proper pumping, and breast milk storage techniques, continued pumping and skin-to-skin care, and expressed breast milk volume increased in our study. PN is associated with complications such as dehydration, electrolyte imbalances, thrombosis, hyperglycemia, hypoglycemia, infection, kidney stones, gallstones, liver failure, and micronutrient deficiencies. Prolongation of PN has risks secondary to starving the gut, growth restriction, infection, and cholestasis.[15] In our study, the total duration of the requirement of PN decreased from 11 days to 7 days after infant feeding quality control policy modification which was beneficial to the newborn.
There is an association between rapid growth during the early postnatal weeks and neurocognitive benefits later in life among preterm and VLBW infants. The postnatal growth pattern in such neonates is often characterized by initial physiological weight loss in the first 7 days of life of approximately 7–15% of their birth weight. Thereafter, recovery occurs with an increase in body weight from around the 10th to the 21st day of life. Poor postnatal growth has a significant bearing on the long-term neurodevelopmental outcome and hence defies the concept of intact survival.[16] In our study, the total time to reach birth weight decreased from 17 days to 11 days after infant feeding quality control policy modification which was beneficial to the newborn.
Kaucher et al. measured maximum milk output with intrusive mechanical methods to extract all the mothers’ milk and reported that production averaged almost 1150 ml/day at 6–10 days postpartum.[17] This level is much higher than the 480–670 ml/day consumed by breastfed infants at the same age.[18] In two separate studies, milk production increased by 15–40% when a breast pump was used to remove additional milk after feedings.[19,20] We also observed that the daily milk output improved to 3 times the baseline amount after the QI. In our study, we observed that QI measures such as expressing milk by breast pump at regular 3rd hourly from the day of delivery, professional health education initiation, establishing breastfeeding guidelines, and maintaining a breast pump dairy can improve the rate of HM production.
Strengths and limitations of the study
A key strength of the present study was that it was generalizable, reliable, and versatile. The PDSA cycle method helped in attending to each QI on a priority basis. One issue with the current study was the lack of a uniform fortification policy in our unit during the study period which could have affected weight gain patterns in the study population. The study was limited in the form of lack of information about coexisting morbidities of prematurity and low birth weight which could have affected weight gain patterns. Moreover, a psychological assessment of mothers including postpartum depression which could have affected maternal lactation was not performed in our study.
CONCLUSION
A simple quality improvement initiative was able to achieve increased lactation in mothers of extreme preterm and VLBW neonates. Implementing the policy of expressing breast milk frequently, breast milk pumping diary, and lactation counseling can increase lactation. By understanding the barriers to breastfeeding, appropriate initiatives can be developed and implemented to facilitate improved breastfeeding practices through such QI projects.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Breastfeeding Report Card-United States 2011. 2011. Atlanta, GA: Centers for Disease Control and Prevention; Available from: http://www.cdc.gov/breastfeeding/pdf/2011breastfeedingreportcard.pdf [Last accessed on 2012 Aug 08]
- [Google Scholar]
- Mucosal immunity: Integration between mother and the breast-fed infant. Vaccine. 2003;21:3382-8.
- [CrossRef] [Google Scholar]
- Evolution of immune functions of the mammary gland and protection of the infant. Breastfeed Med. 2012;7:132-42.
- [CrossRef] [PubMed] [Google Scholar]
- Initiation and continuation of breastfeeding: Theory of planned behavior. J Adv Nurs. 2005;50:272-82.
- [CrossRef] [PubMed] [Google Scholar]
- Mothers' stories about their experiences in the neonatal intensive care unit. Neonatal Netw. 2000;19:13-21.
- [CrossRef] [PubMed] [Google Scholar]
- Antiinfective properties of human milk. J Nutr. 2008;138:1801s-6s.
- [CrossRef] [PubMed] [Google Scholar]
- Protection of the neonate by the innate immune system of developing gut and of human milk. Pediatr Res. 2007;61:2-8.
- [CrossRef] [PubMed] [Google Scholar]
- Breastfeeding the high-risk infant: Implications for midwifery management. J Midwifery Womens Health. 2000;45:238-45.
- [CrossRef] [Google Scholar]
- The impact of prematurity and neonatal illness on the decision to breastfeed. J Adv Nurs. 1997;25:729-37.
- [CrossRef] [PubMed] [Google Scholar]
- Awareness of breastfeeding recommendations and duration of breastfeeding: Findings from the healthy beginnings trial. Breastfeed Med. 2012;7:223-9.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of employment status on breastfeeding in the United States. Womens Health Issues. 2006;16:243-51.
- [CrossRef] [PubMed] [Google Scholar]
- Delayed initiation of breast-feeding the preterm infant. J Perinat Neonatal Nurs. 1995;9:10-20.
- [CrossRef] [PubMed] [Google Scholar]
- Breastfeeding rates of VLBW infants In: Koletzko B, Michaelsen KF, Hernell O, eds. Short and Long Term Effects of Breast Feeding on Child Health Advances in Experimental Medicine and Biology. Vol 478. Boston, MA: Springer; 2002.
- [Google Scholar]
- The rush mothers' milk club: Breastfeeding interventions for mothers with very low birth weight infants. J Obstet Gynecol Neonatal Nurs. 2004;33:164-74.
- [CrossRef] [PubMed] [Google Scholar]
- Complications associated with parenteral nutrition in the neonate. Clin Perinatol. 2014;41:331-45.
- [CrossRef] [PubMed] [Google Scholar]
- Postnatal growth in VLBW infants: Significant association with neurodevelopmental outcome. J Pediatr. 2003;143:163-70.
- [CrossRef] [Google Scholar]
- Human milk studies. XX The diet of lactating women and the collection and preparation of food and human milk for analysis. Am J Dis Child. 1945;70:142-7.
- [CrossRef] [PubMed] [Google Scholar]
- Nutrient intake by breastfed infants during the first five days after birth. Am J Dis Child. 1986;140:933-6.
- [CrossRef] [PubMed] [Google Scholar]
- Infant self-regulation of breast milk intake. Acta Paediatr Scand. 1986;75:893-8.
- [CrossRef] [PubMed] [Google Scholar]
- Is maternal milk production limiting for infant growth during the first year of life in breastfed infants? In: Goldman AS, Atkinson SA, Hanson LA, eds. Human Lactation 3: The Effects of Human Milk on the Recipient Infant. New York: Plenum Press; 1987. p. :123-33.
- [CrossRef] [Google Scholar]






