Translate this page into:
Intracranial epidermoid lesions: Our experience of 56 cases
*Corresponding author: Anmol Singh Randhawa, Department of Neurosurgery, Mahatma Gandhi University of Medical Sciences and Technology, Jaipur, Rajasthan, India. randhawa.anmol@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Sherpa TD, Randhawa AS, Srivastava A, Agrawal S, Jain PK, Agrawal Y, et al. Intracranial epidermoid lesions: Our experience of 56 cases. Sri Ramachandra J Health Sci. 2024;4:59-64. doi: 10.25259/SRJHS_6_2024
Abstract
Objectives
This study aims to present a case series evaluating the clinical presentation and surgical outcomes in patients diagnosed with intracranial epidermoid lesions.
Material and Methods
From January 2015 to December 2022, a 7-year retrospective analysis was carried out at the Mahatma Gandhi Hospital’s Department of Neurosurgery in Jaipur.
Results
The study comprised 56 patients who had surgery to remove cerebral epidermoid lesions. These included 39 with infratentorial lesions and 17 with supratentorial lesions. The most prevalent symptom, affecting 40 patients, was a headache. Seizures occurred in 14 patients with supratentorial lesions. Twenty-four patients with cerebellopontine (CP) angle lesions had trigeminal neuralgia symptoms, whereas patients with suprasellar epidermoid lesions mainly complained of headaches and visual abnormalities. Three individuals having CP angle tumors experienced post-operative facial weakness; two of these patients experienced temporary facial weakness, while one patient experienced persistent facial weakness. Patients with suprasellar epidermoid lesions showed post-operative improvement in visual impairment, though four required hormonal replacement therapy. In addition, one patient experienced a cerebrospinal fluid leak, and three patients developed post-operative meningitis.
Conclusion
Intracranial epidermoid lesions can occur in various locations within the skull. They usually exhibit symptoms associated with elevated intracranial pressure and particular neurological impairments, depending on their location, just like other space-occupying lesions. With a minimal incidence of complications, surgical results for these lesions generally turn out positive.
Keywords
Cerebellopontine angle
Complication
Epidermal lesion
Surgical outcome
INTRODUCTION
About 1% of all brain tumors are intracranial epidermoid lesions, which are non-cancerous.[1] These lesions originate from ectodermal cells that fail to differentiate properly during weeks three through five of fetal development, coinciding with the formation in the neural tube. Approximately 90% of intra-cranial epidermoids are found in the intradural compartment. However, they can also be found in extradual compartments, in the intradiploic space of the frontal, parietal, temporal, and occipital bones.[2,3] Epidermoid lesions are most often found in the brain’s suprasellar regions, temporal region, and cerebellopontine (CP) angle.[4] As with other intracranial masses, they can cause symptoms related either neurological impairments or elevated intracranial pressure as a result of the pressure exerted on brain structures or cranial nerves. For instance, in the suprasellar region, patients may experience vision problems, whereas those with temporal lobe lesions might suffer from seizures. Lesions in the CP angle frequently exhibit numbness and facial pain.
Patients frequently seek medical attention late in the course of the disease because epidermoid lesions grow very slowly,[5] which causes a lengthy time before symptoms become apparent.[6] Diffusion-weighted magnetic resonance imaging (MRI), in particular, is essential for diagnosing these lesions and distinguishing them from arachnoid cysts. Surgery remains the most effective treatment, with generally favorable outcomes. However, the tumors are often adherent to surrounding tissues, leaving residual fragments that may cause recurrence.[7] In addition, the surgical removal of these lesions carries a risk of chemical meningitis due to irritation from the cystic contents. Although complete surgical resection is the goal, it is sometimes unachievable without causing significant neurological damage.[8]
Given the rarity of intracranial epidermoid lesions, information about their post-surgical outcomes is limited. This study seeks to assess the clinical outcomes of patients who underwent surgical treatment for these lesions.
In this research, we looked at the histology, neuroradiological results, as well as clinical symptoms of 56 intracranial epidermoid patients who had surgery in Mahatma Gandhi Hospital between the years 2015 and 2022. In addition, we documented instances with a poor prognosis and identified any post-operative problems. The patients were followed up for a period of 6 months on average.
MATERIAL AND METHODS
From January 2015 to December 2022, the present retrospective investigation was carried out in the neurosurgery department of Mahatma Gandhi Hospital in Jaipur. In all, 56 patients diagnosed with intracranial epidermoid lesions were included in the study, excluding those with recurrence. Depending on the location of the lesion, patients underwent either a craniotomy or craniectomy. In most cases, total resection of the lesion was achieved. After surgery, patients were given 1 g of ceftriaxone twice day and 4 mg of dexamethasone 3 times daily for 3 days, while the surgical site was irrigated with saline. Medical history, clinical presentation, imaging results, and histology were among the patient data that were gathered in the past and examined with the Statistical Package for the Social Sciences version 20.
Inclusion criteria
All patients diagnosed with intracranial epidermoid lesions based on pre-operative radiological findings
Patients aged 11 years and above
Patients treated between January 2015 and December 2022 at Mahatma Gandhi Hospital’s Neurosurgery Department in Jaipur
Patients with complete and accessible medical records, including clinical presentation, imaging findings, operative details, and post-operative follow-up data.
Exclusion criteria
Non-epidermoid lesions
Patients presenting with recurrent epidermoid lesions that had previously been treated surgically
Patients without sufficient post-operative follow-up data or those lost to follow-up
Patients with severe systemic illnesses or other conditions that significantly affect their surgical outcome and clinical course.
RESULTS
The male-to-female ratio of the 56 patients in the study was 1:1.1, with 27 of them being male and 29 being female. The average age was 36, with a range of 11–66 years [Table 1 and Figure 1].
| Gender | Number (years) |
|---|---|
| Male | 27 |
| Female | 29 |
| Mean age | 36 |
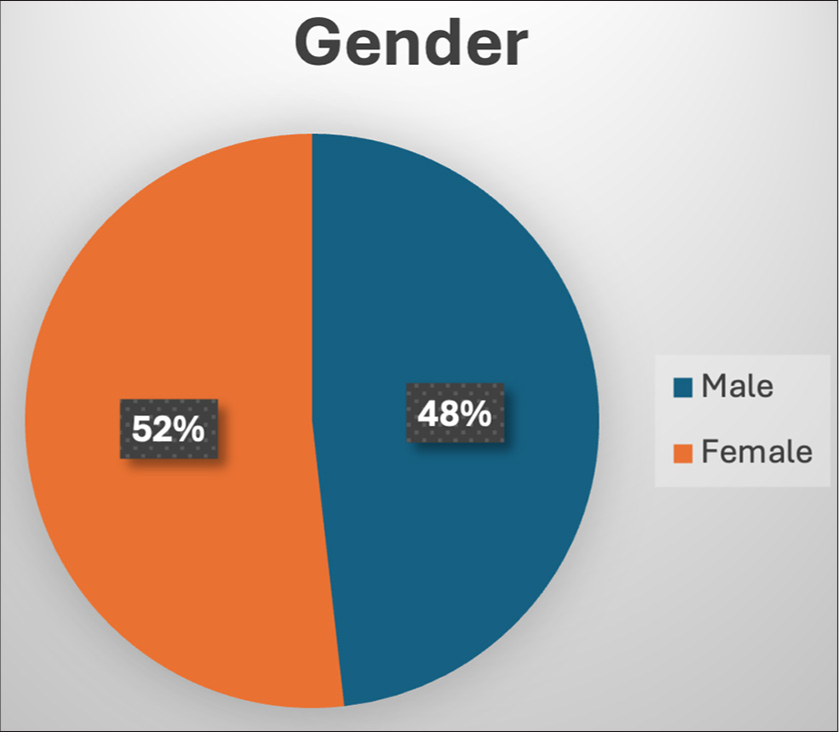
- Age distribution.
A total of 18 patients presented with supratentorial lesions, while 37 had infratentorial lesions. Among the supratentorial cases, two patients had four lesions in the temporal lobe, four throughout both suprasellar or parasellar regions [Figure 2a and b], and one lesion that extended into the parietal lobe or cavernous sinus. In addition, four patients had lesions in the sphenoid wing and sphenoidal region, and three in the interhemispheric cistern [Figure 3a and b]. Most of the infratentorial lesions were located in the CP angle, with 31 cases reported [Figure 4a and b]. Other infratentorial locations included the pineal region in four patients [Figure 5a and b], as well as the quadrigeminal cistern and the fourth ventricle, each observed in two patients [Table 2 and Figure 6]. Out of the total patients, 40 presented with headaches, 14 experienced seizures, and 24 trigeminal neuralgia symptoms were observed in patients with lesions at the CP angle. Visual field deficits were present in all patients with parasellar and suprasellar epidermoid lesions, three patients having sphenoid wing lesions, and two patients with temporal lobe lesions. Four of these patients also exhibited hormonal deficiencies: two had a cortisol shortage alone, and two had a thyroid and cortisol deficiency. One patient had tumor extension to a cavernous sinus, leading to third and sixth cranial nerve palsy, and four individuals with epidermoid lesions within the frontotemporal region showed mild paralysis as a result of tumor involvement in the motor strip [Table 3].
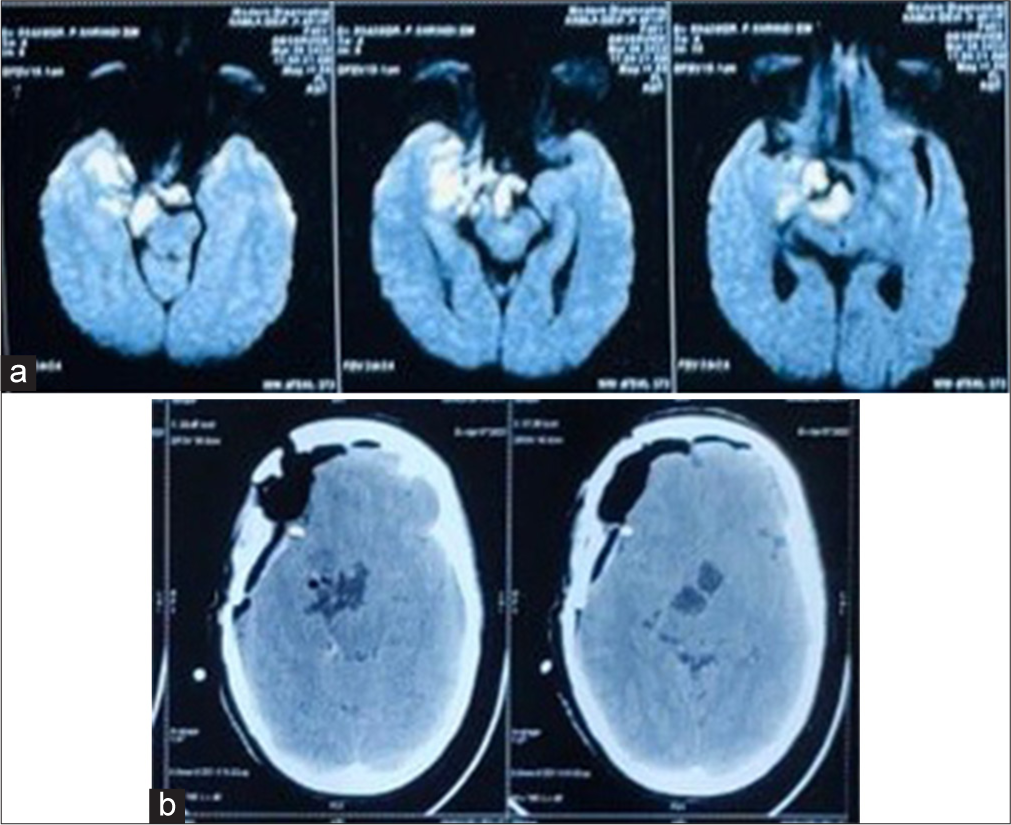
- (a) On the diffusion-weighted image, the parasellar region shows a high-intensity signal. (b) Post-operative computed tomography brain.
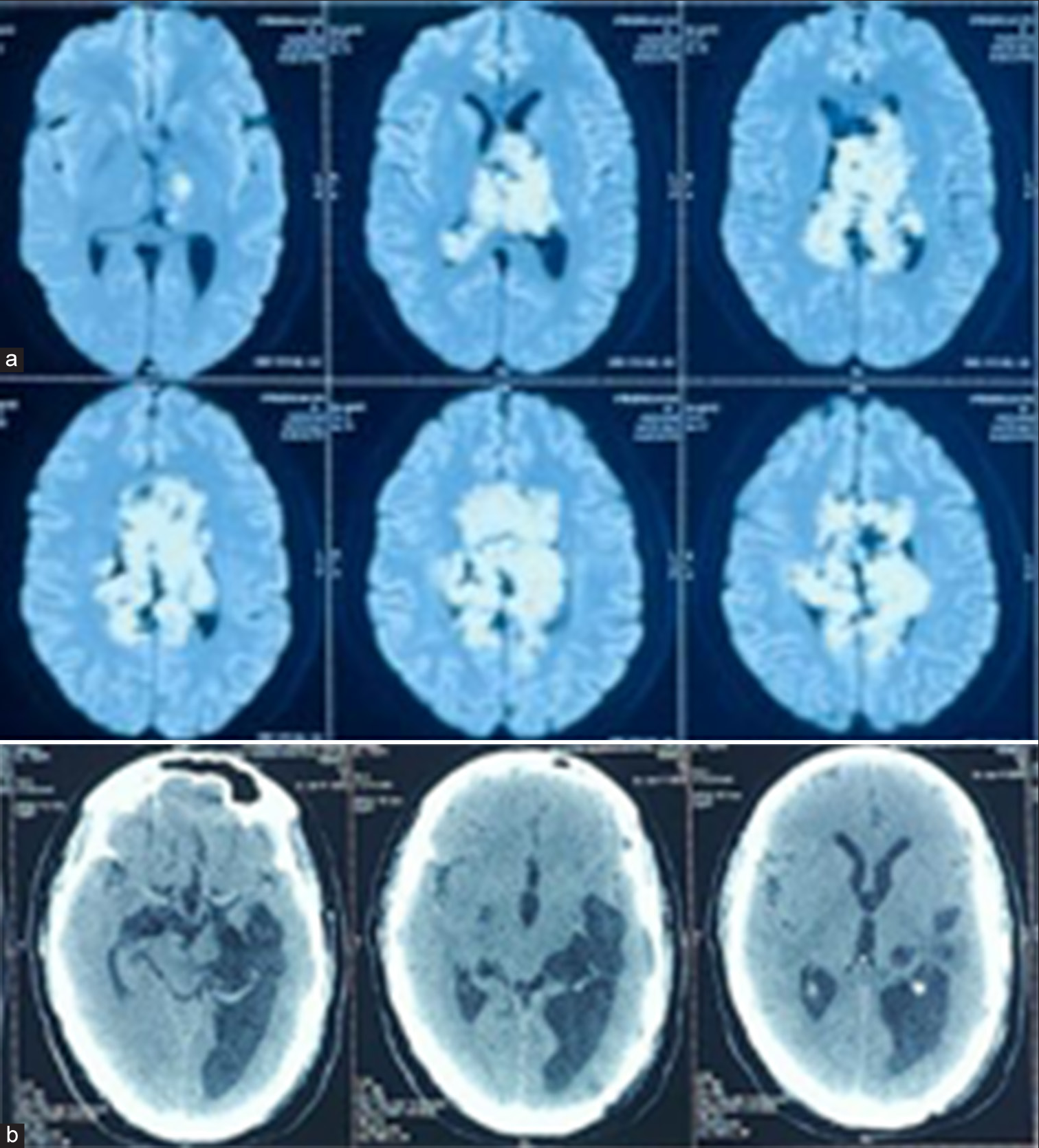
- (a) On the diffusion-weighted image, the interhemispheric area shows a high-intensity signal. (b) Post-operative computed tomography brain.
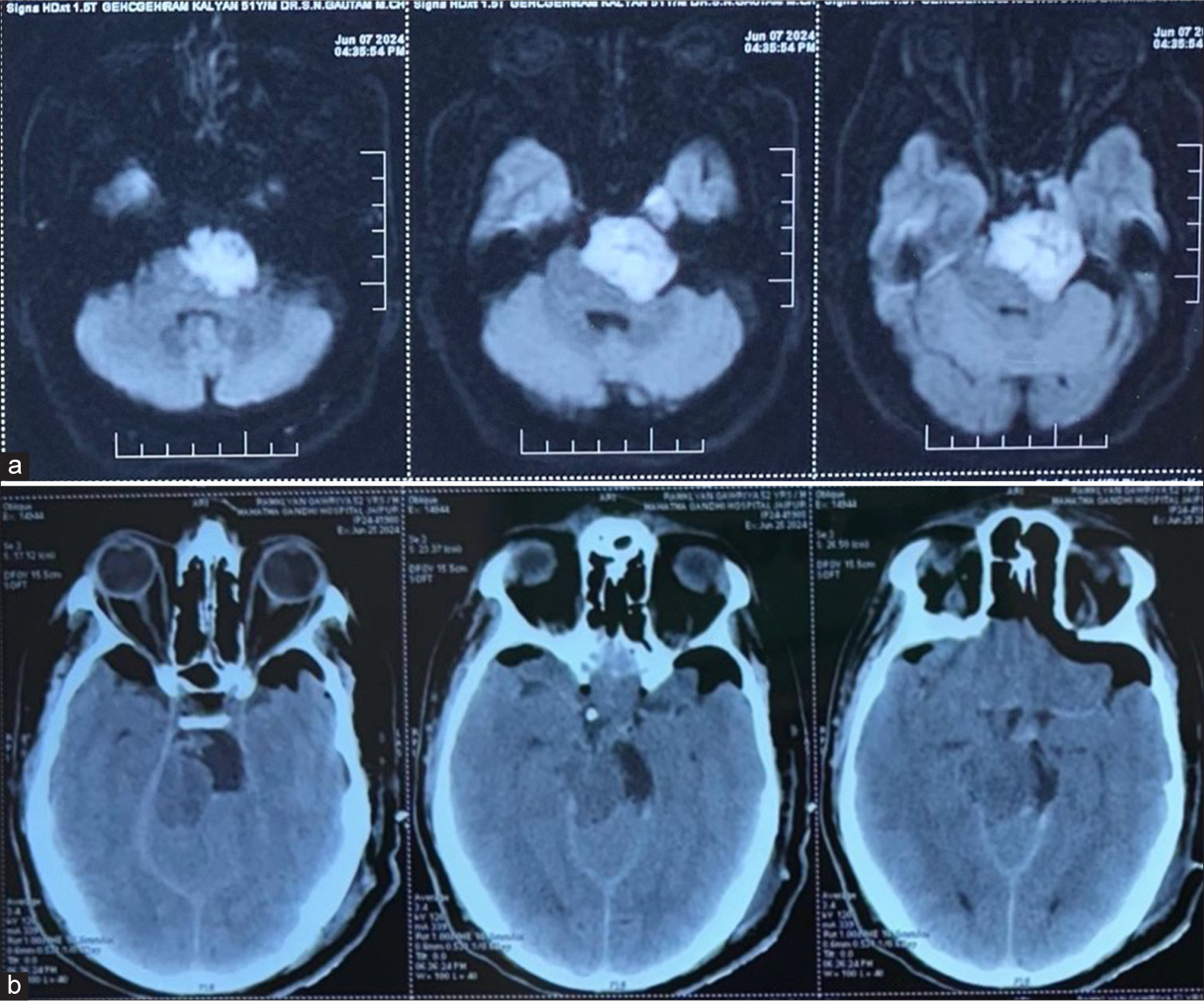
- (a) Diffusion-weighted pre-operative brain magnetic resonance imaging revealed a diffusion restriction in the left cerebellopontine angle. (b) Post-operative computed tomography brain.
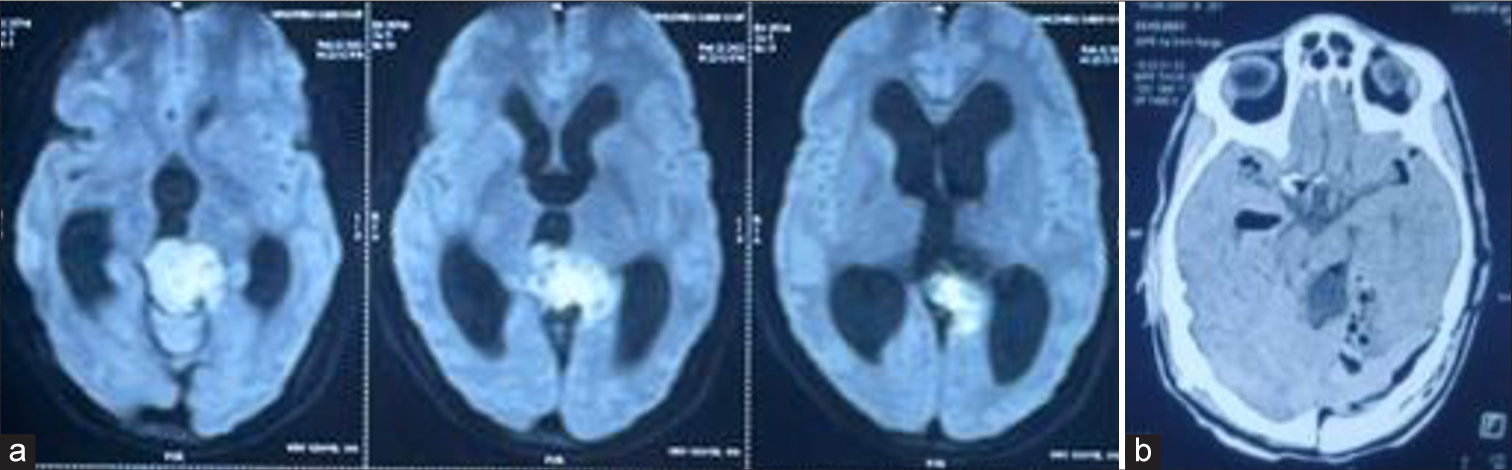
- (a) On the diffusion-weighted image, the pineal region shows a high-intensity signal. (b) Post-operative computed tomography brain.
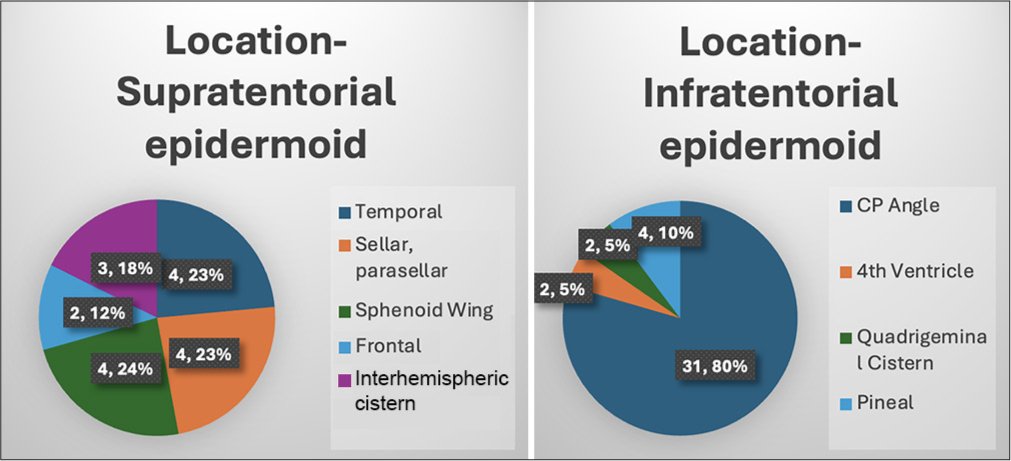
- Location-wise distribution. CP: Cerebellopontine angle
| Location | Number |
|---|---|
| Supra-tentorial | 17 |
| Temporal | 4 |
| Sellar, parasellar | 4 |
| Sphenoid wing | 4 |
| Frontal | 2 |
| Interhemispheric | 3 |
| Infra-tentorial | 39 |
| 4th ventricle | 2 |
| CP angle | 31 |
| Quadrigeminal cistern | 2 |
| Pineal | 4 |
CP: Cerebellopontine angle
| Complaints | Number |
|---|---|
| Headache | 40 |
| Seizures | 14 |
| Trigeminal neuralgia | 24 |
| Dysphagia, lower cranial nerve palsy | 8 |
| Visual and field defects | 9 |
| Motor weakness | 4 |
| Hormonal deficiency | 4 |
All patients in the study underwent surgical intervention. Three individuals having CP angle tumors experienced facial palsy after surgery. After 4 months, one of these patients exhibited no progress, while the other two recovered. After surgery, all patients with suprasellar epidermoids experienced improvements in their visual field abnormalities.
Nevertheless, following surgery, four individuals with suprasellar malignancies needed hormone replacement treatment. Three patients experienced post-operative meningitis following surgery, and one patient experienced cerebrospinal fluid (CSF) leaking. Rest of the patients all experienced improvement in pre-operative symptoms [Table 4].
| Complications | Number |
|---|---|
| CSF leak | 1 |
| Diplopia | 2 |
| Meningitis | 3 |
| Facial palsy | 3 |
CSF: Cerebrospinal fluid
In our study, 51 patients (91.1%) underwent gross total or near-total resection of their epidermal lesions [Table 5]. This is generally preferred as it offers the best chance for preventing recurrence and improving long-term outcomes. Complete removal of the lesion is crucial, especially considering the slow-growing nature of epidermoid tumors, which can cause significant mass effects over time if not fully excised. However, in 5 patients (8.9%), only a subtotal resection was possible. Subtotal resections are sometimes necessary when the lesion is closely associated with essential components, including the brainstem or cranial nerves. In these cases, preserving neurological function takes precedence, and complete resection may carry a higher risk of morbidity. While subtotal resection increases the likelihood of recurrence, it is often a safer option to prevent severe complications during surgery.
| Resection | Number (Percentage) |
|---|---|
| Gross total resection/near-total resection | 51 (91.1) |
| Subtotal resection | 5 (8.9) |
DISCUSSION
Intracranial epidermoid lesions are congenital anomalies that grows very slowly. Most patients remain asymptomatic, with only a few developing noticeable symptoms.[9] When symptoms do arise, they are typically due to the gradual pressure exerted by the growing lesion. Common signs include seizures, cerebellar abnormalities, headaches, or cranial nerve dysfunction.[10] The gradual expansion of these lesions means that symptoms often present late, typically between the ages of 20 and 40, which aligns with our study’s finding of an average patient age of 36 years.[11,12] When it comes to making a pre-operative diagnosis of epidermoid lesions, radiological imaging is essential. To differentiate these lesions from arachnoid cysts, which do not restrict due to the existence of free water molecules,[5] they usually appear as low-density masses on computed tomography scans[13] or exhibit restricted diffusion on diffusion-weighted imaging (DWI) on MRI. In approximately 25% of instances, there is minor rim enhancement, which is probably caused by peritumoral granulation from cyst leaking, even though the majority of epidermoid lesions have no improvement with contrast.[14] We were more confident in the pre-operative diagnosis because all of the patients in our research showed restricted diffusion on DWI. Most intracranial epidermoid lesions[15] occur in the CP angle, which accounts for 5–10% of all CP angle tumors and is present in 40–50% of patients. Consistent with earlier findings, 31 out of 56 patients (55%) in our study exhibited lesions in the CP angle. In line with documented examples, these patients most commonly reported trigeminal neuralgia and hearing loss.[7]
Other common locations for intracranial epidermoid lesions comprise the parasellar areas (10–15%), the 4th ventricle (17%), or, less frequently, the brainstem and cerebral hemispheres.[9] Frontal lobe epidermoid lesions are rare and usually manifest with seizures.[16] In our study, both patients with frontal lobe epidermoids experienced seizures and neurological deficits. While temporal lobe epidermoid tumors are considered rare, our series included four cases, suggesting these tumors may be more prevalent than previously believed. Due to their uneven, lobulated surfaces and propensity to cling to or enclose nearby arteries and nerves, epidermoid cysts can be difficult to remove surgically. The involvement of vital components such as the brainstem or cranial nerves makes complete excision frequently challenging. There is a significant risk of morbidity even though complete resection offers the best chance of preventing recurrence and guaranteeing a normal life expectancy.[4] Thus, to maintain neurological function, subtotal resection may occasionally be required.[17,18]
In our study, the rate of complications following surgery was 12.5% (seven out of 56 patients), consistent with previously reported rates.[19,20] Before the advent of microsurgical techniques, mortality rates from surgery ranged from 20% to 57%. However, with advances in neuroimaging and microsurgery, the mortality rate has significantly decreased, and no deaths were recorded in our case series.
Post-operative meningitis occurred in three of our patients; however, it is unclear if this was caused by germs or chemicals, as the latter is a known side effect of epidermoid tumors. The discharge of cystic acid can cause chemical aseptic meningitis. Leading to an inflammatory response ranging from mild leptomeninges to more severe conditions such as granulomatous meningitis and epididymitis. Given the similarity in spinal fluid profiles between bacterial and chemical meningitis, it is safer to initiate antibiotic therapy early to cover both possibilities.[21]
Although hydrocephalus is considered uncommon in patients with epidermoid lesions due to the slow growth of the lesion and the permeable nature of CSF around the lesion, three of our patients required pre-operative CSF diversion procedures (ventriculoperitoneal shunts). Two additional patients required post-operative shunt placement. Twelve of thirty individuals who had CP angle epidermoid required shunt surgery for hydrocephalus in a previously published dataset.[22]
CONCLUSION
Anywhere in the brain, epidermoid lesions can develop gradually, which are benign. Clinical appearance frequently shows signs of elevated intracranial pressure or focal neurological impairments brought on by the tumor’s local mass effect. The goal of surgery is total resection, and recovery is great with few post-operative complications after resection.
Acknowledgment
We would like to thank the Departments of Neurosurgery and Radiology for providing us with the necessary data for this study to be conducted and our Head of Department for guiding and motivating us to conduct this study.
Ethical approval
Institutional Review Board approval is not required as it is a retrospective study.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Intracranial epidermoid cyst with hemorrhage: MR imaging findings. Am J Neuroradiol. 2006;27:427-9.
- [Google Scholar]
- Radiologic-pathologic correlation. Epidermoid tumor of the cerebellopontine angle. AJNR Am J Neuroradiol. 1992;13:863-82.
- [CrossRef] [PubMed] [Google Scholar]
- Intracranial epidermoid cysts: Benign entities with malignant behavior: Experience with 36 cases. Sci Rep. 2023;13:6474.
- [CrossRef] [PubMed] [Google Scholar]
- Intracranial epidermoid tumor; microneurosurgical management: An experience of 23 cases. Asian J Neurosurg. 2013;8:21-8.
- [CrossRef] [PubMed] [Google Scholar]
- Diffusion tensor mode in imaging of intracranial epidermoid cysts: One step ahead of fractional anisotropy. Neuroradiology. 2009;51:123-9.
- [CrossRef] [PubMed] [Google Scholar]
- Hypertrophic cranial pachymeningitis after Mollaret's Meningitis: Case report and review of the literature. J Neurol Sci (Turk). 2007;24:331-7.
- [Google Scholar]
- Clinical presentation of intracranial epidermoids: A surgical series of 20 initial and four recurred cases. Asian J Neurosurg. 2010;5:32-40.
- [Google Scholar]
- Cerebellopontine angle epidermoids presenting with cranial nerve hyperactive dysfunction: Pathogenesis and long-term surgical results in 30 patients. Neurosurgery. 2002;50:276-85.
- [CrossRef] [PubMed] [Google Scholar]
- Epidermoid tumors of the temporal lobe as epileptogenic foci. J Clin Neurosci. 2011;18:1396-9.
- [CrossRef] [PubMed] [Google Scholar]
- Cerebellopontine angle epidermoid cysts: A report on 30 cases. J Neurol Neurosurg Psychiatry. 1989;52:986-90.
- [CrossRef] [PubMed] [Google Scholar]
- Microneurosurgical treatment of intracranial dermoid and epidermoid tumors. Neurosurgery. 1989;24:561-7.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical treatment of parapontine epidermoid cysts presenting with trigeminal neuralgia. J Clin Neurosci. 2011;18:344-6.
- [CrossRef] [PubMed] [Google Scholar]
- An unusual middle fossa interdural epidermoid tumor. Case report. J Neurosurg. 2001;95:902-4.
- [CrossRef] [PubMed] [Google Scholar]
- Intracranial cysts: Radiologic-pathologic correlation and imaging approach. Radiology. 2006;239:650-64.
- [CrossRef] [PubMed] [Google Scholar]
- Intraparenchymal epidermoid cyst of the right frontal lobe: A case report. No Shinkei Geka. 1985;13:695-9.
- [Google Scholar]
- Clinical characteristics and diagnostic imaging of epidermoid tumors. J Clin Neurosci. 2011;18:1158-62.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical treatment of epidermoid cysts of the cerebellopontine angle. J Neurosurg. 1996;84:14-9.
- [CrossRef] [PubMed] [Google Scholar]
- Surgery of intracranial epidermoid cysts. Report of 44 patients and review of the literature. Neurochirurgie. 2002;48:5-13.
- [Google Scholar]
- Recurrent meningitis due to epidermoid. J Pediatr Neurosci. 2012;7:47-8.
- [CrossRef] [PubMed] [Google Scholar]
- Experience with cerebellopontine angle epidermoids. Neurosurgery. 1997;40:24-9.
- [CrossRef] [PubMed] [Google Scholar]






