Translate this page into:
Role of IL-6 as ‘core inflammatory marker’ in assessment of severity, response to therapy and predicting outcome in COVID-19 pneumonia: A single center experience of 2400 cases in tertiary care setting in India
*Corresponding author: Shital Patil, Department of Pulmonary Medicine, Maharashtra Institute of Medical Sciences and Research Medical College, Venkatesh Chest Hospital, Latur, Maharashtra, India. drsvpatil1980@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Patil S, Patil D, Khule S. Role of IL-6 as ‘core inflammatory marker’ in assessment of severity, response to therapy and predicting outcome in COVID-19 pneumonia: A single center experience of 2400 cases in tertiary care setting in India. Sri Ramachandra J Health Sci. 2023;3:60-7. doi: 10.25259/SRJHS_17_2022
Abstract
Objectives:
In coronavirus disease-19 (COVID-19) pneumonia, the role of various inflammatory markers including interleukin-6 (IL-6) was evolved in managing cases in indoor or critical care units worldwide. Apart from the role of IL-6 in predicting cytokine storms, the role in assessing post-COVID outcome is less studied. In the present study, we have analyzed the role in predicting ventilatory support requirement and final outcome in COVID-19 pneumonia.
Material and Methods:
A prospective, observational, and 12 weeks follow-up study included 2400 COVID-19 cases confirmed with reverse transcription-polymerase chain reaction. All cases were assessed with lung involvement documented and categorized on high-resolution computerized tomography (HRCT) thorax, oxygen saturation (SpO2), and IL-6 at entry point and follow-up. Covariates such as age, gender, and comorbidity; interventions such as oxygen use, bi-level positive airway pressure/non-invasive ventilation (BIPAP/NIV); and timings of ventilatory support and final outcome as with or without lung fibrosis as per computed tomography severity were recorded. Covariates were analyzed with initial and sequential IL-6 titer. Statistical analysis is done by Chi-square test.
Results:
The study of 2400 COVID-19 pneumonia cases, age (<50 and >50 years), gender, and comorbidity has a significant association with IL-6 titer (P < 0.00001). HRCT severity score at entry point and duration of illness has a significant correlation with IL-6 level (P < 0.00001). IL-6 titer has a significant association with SpO2 and BIPAP/NIV requirement during hospitalization (P < 0.00001). Timing of BIPAP/NIV requirement during the course of hospitalization in the intensive care unit has a significant association with IL-6 titer (P < 0.00001). Follow-up IL-6 titer during hospitalization as compared to entry point normal and abnormal IL-6 has a significant association in post-COVID lung fibrosis (P < 0.00001). Follow-up IL-6 titer during hospitalization as compared to entry point abnormal IL-6 has a significant association in predicting cytokine storms irrespective of normal or abnormal IL-6 at entry point (P < 0.0001).
Conclusion:
IL-6 titer has documented a very important role in triaging the COVID-19 pneumonia cases in indoor units, and guided treatments have shown improved outcomes. IL-6 titer is the “game changer” inflammatory marker not only in assessing the severity or predicting course during hospitalization but it has also helped in the utilizations of timely interventions required during hospitalizations. Sequential IL-6 titer has shown a significant role in predicting final radiological outcomes at 12 weeks.
Keywords
Coronavirus disease-19 pneumonia
Interleukin-6
Oxygen saturation
Inflammatory marker
INTRODUCTION
Coronavirus disease-19 (COVID-19) is first coronavirus-related global pandemic caused by novel severe acute respiratory syndrome coronavirus-2, and rapid evolution of the pandemic has resulted in fast-track developments in antivirals, medical management, and vaccination for use to prevent morbidity and mortality. Although lung is the primary target organ involved in COVID-19, many patients were having pulmonary and extrapulmonary manifestations of diseases variably as resultant pathophysiological effects of the immune activation pathway and direct virus-induced lung damage. In COVID-19 pneumonia, pathophysiology constitutes different pathways such as immune activation, inflammatory, thrombogenic, and direct viral infection to lungs, and extrapulmonary tissues.[1]
Although the majority of published data has included, severe COVID-19 cases with critical illness hospitalized in indoor units and analyzed single time point interleukin-6 (IL-6) titer using cross-sectional studies rather than prospective and repeated or sequential titer measurement studies.[2-4] This indicates a major gap in understanding the significant impact of these inflammatory markers in the overall assessment of COVID-19 pneumonia in those cases with clinical deterioration occurs, which can be earliest picked up by doing sequential IL-6 titers.[5-7]
Importantly, different inflammatory biomarkers such as C-reactive protein (CRP), ferritin, lactate dehydrogenase (LDH), and D-dimer have documented important role in analyzing severity, predicting the need of interventions, targeting treatment options, and predicting the final outcome in COVID-19 pneumonia along with IL-6 titers.[8-10] Authors have documented the important role of these inflammatory markers in overall predicting outcomes, and all these markers have been done in a quantified manner in hospitalized COVID-19 cases and followed cases till 3 months of discharge from the hospital.[11-15]
As per published voidance, IL-6 is superior to CRP and other inflammatory markers in predicting ongoing inflammation and a better tool to predict cytokine storms and cases with impending respiratory failure. IL-6 is the most important driver of immune dysregulation, and its impact has been shown in acute respiratory distress syndrome (ARDS) and respiratory failure in COVID-19 disease.[5-7]
In the present study, we have analyzed the role of IL-6 in COVID-19 pneumonia with special emphasis on the need for ventilatory support in correlation with IL-6 titer and the impact of these sequential titers of IL-6 in predicting final radiological outcomes.
MATERIAL AND METHODS
Data source
This study was approved by the Institutional Review Board/ Ethics Committee at Venkatesh Hospital and Critical Care Center Latur India and Maharashtra Institute of Medical Sciences and Research (MIMSR) Medical College Latur India, (Approval # VCC/119-2020-2021; Approval date 22/11/2020).
Methodology
A prospective and observational study, conducted during July 2020–June 2021, in MIMSR Medical College and Venkatesh Hospital Latur India, included that 2400 COVID-19 cases confirmed with reverse transcription-polymerase chain reaction (RT-PCR), to find out the role of IL-6 in predicting the severity of illness, assessing response to therapy and outcome as post-COVID fibrosis in diagnosed COVID-19 pneumonia cases admitted in the critical care unit. A total 2400 cases were enrolled in the study after written and informed consent was obtained from all individual participants admitted in indoor units after assessing overall status to give consent and whenever required, taken from attendants of critically ill admitted cases [Figure 1].
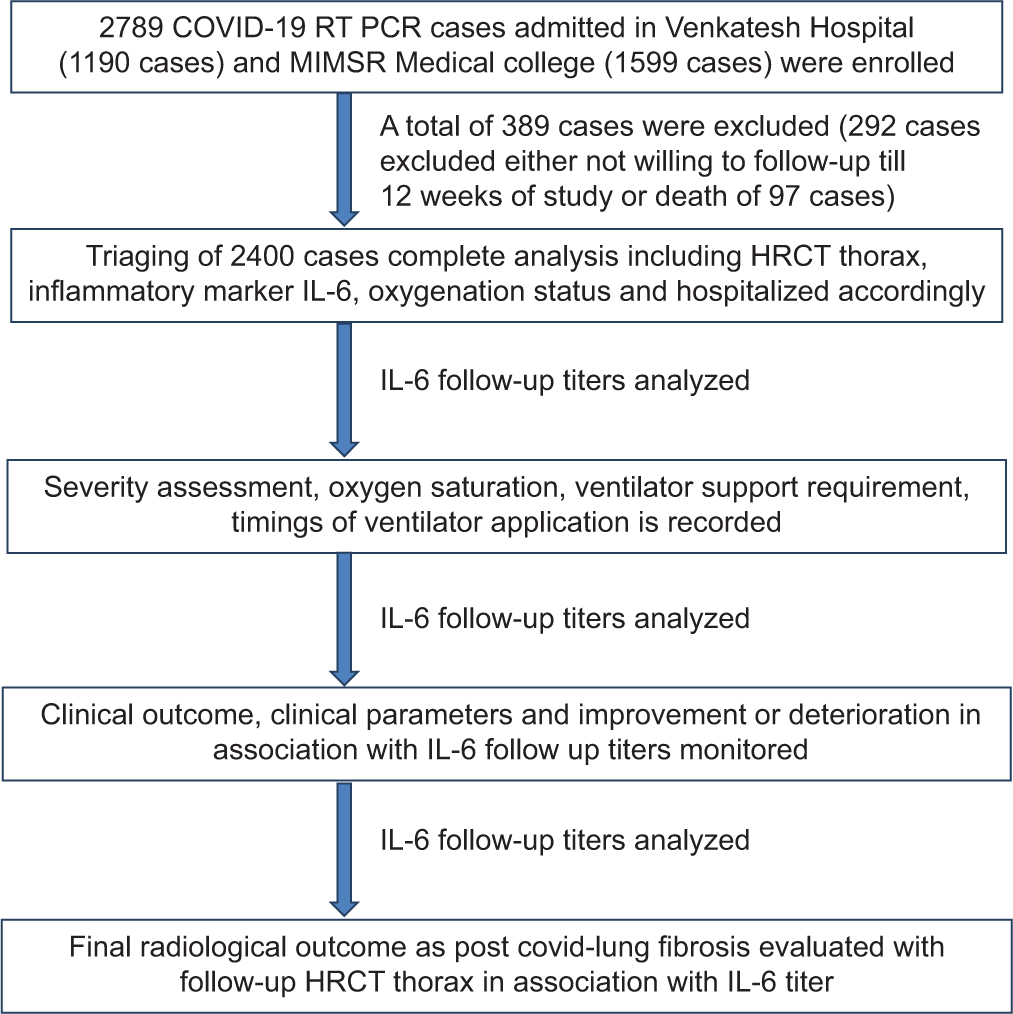
- Flow of the study.
Inclusion criteria
COVID-19 patients, confirmed with RT-PCR, above the age of 18 years, hospitalized in the study centers, including those with comorbidities and irrespective of severity and oxygen saturation (SpO2) was included in the study.
Exclusion criteria
Those not willing to give consent, not able to perform IL-6, and not willing to remain in follow-up were excluded from the study.
Study design
All study cases underwent the following assessment before enrolling in the study
COVID-19 RT-PCR test was performed on nasopharyngeal samples collected with all standard institutional infection control policies and enrolled all cases with positive COVID-19 RT-PCR test.
High-resolution computerized tomography (HRCT) thorax to assess the severity of lung involvement as per COVID-19 reporting and data system,[16] and categorized as mild if score <7, moderate if score 8–15, and severe if score >15 or 15–25.
Clinical assessment and routine biochemistry and hematological workup with viral inflammatory markers as CRP, ferritin, LDH, and IL-6 titers.
Entry point IL-6 titer was utilized as an assessment tool of the severity of illness with clinical parameters. If IL-6 analysis was normal at the entry point, then IL-6 titer was repeated on the day of discharge from the hospital or done during hospitalization if the clinical course deteriorated. If IL-6 analysis was abnormal at the entry point, we repeated it every 72 h as a follow-up to assess the severity, progression of illness, and titer level utilized to assess response to medical treatment.
Follow-up HRCT thorax was done after 12 weeks or 3 months of discharge from the hospital for analysis of post-COVID lung fibrosis in selected cases with abnormal IL-6 level at discharge and required bi-level positive airway pressure/non-invasive ventilation (BIPAP/NIV) during hospitalization and cases required oxygen supplementation at home [Figure 1].
Methodology of IL-6 titer assessment: Immunoturbidimetry
Normal values
Normal values up to <7 pg/mL.
Interpretation of results
Negative: Value up to <7 pg/mL[17]
Positive: Value above >7 pg/mL[17]
Significant: Four-fold raised IL-6 vale, that is, >28 pg/mL
Highly significant: Sixteen-fold raised values, that is, 98 pg/mL, that is, level considered as required for labeled as cytokine storm
Follow-up significance: Values raised or decreased in two-to-four-fold change.
Statistical analysis
The statistical analysis was done using Chi-square test in R-3.4 software. Significant values of χ2 were seen from the probability table for different degrees of freedom required. P-value was considered significant if it was below 0.05 and highly significant in case it was <0.001.
RESULTS
Covariates
In the present study, 2400 COVID-19 pneumonia cases confirmed by COVID-19 RT PCR, males were 1431/2400 and females were 969/2400, age >50 were 1563 cases, and age <50 were 837 cases. Significant association in IL-6 and COVID-19 pneumonia has been documented with variables such as age, gender, diabetes mellitus, IHD, hypertension, COPD, and obesity (P < 0.00001) [Table 1].
| COVID-19 RT-PCR positive (n=2400) | IL-6 level normal (n=990) | IL-6 level abnormal (n=1410) | Chi-square test value and Pvalue |
|---|---|---|---|
| Age>50 years (n=1563) | 331 | 1232 | χ2=745.12 |
| Age<50 years (n=837) | 659 | 178 | P<0.00001 |
| Male gender (n=1431) | 667 | 764 | χ2=42.02 |
| Female gender (n=969) | 323 | 646 | P<0.00001 |
| Diabetes mellitus (n=1398) | 349 | 1049 | χ2=366.46 |
| Without diabetes (n=1002) | 641 | 361 | P<0.00001 |
| Hypertension (n=471) | 81 | 390 | χ2=139.89 |
| Without hypertension (n=1929) | 909 | 1020 | P<0.00001 |
| COPD (n=239) | 56 | 183 | χ2=34.77 |
| Without COPD (n=2161) | 934 | 1227 | P<0.00001 |
| IHD (n=339) | 108 | 239 | χ2=16.70 |
| Without IHD (n=2061) | 882 | 1179 | P<0.000056 |
| Obesity (n=272) | 91 | 181 | χ2=7.68 |
| Without obesity (n=2128) | 899 | 1229 | P<0.005554 |
IL-6: Interleukin-6, COVID-19: Coronavirus disease-19, RT-PCR: Reverse transcription polymerase chain reaction, COPD: Chronic obstructive pulmonary disease, IHD: Ischemic heart disease
Core observations
HRCT severity score at entry point with IL-6 level has a significant correlation in COVID-19 pneumonia cases (P < 0.00001) [Table 2]. IL-6 level has a significant association with duration of illness (Doi) in COVID-19 pneumonia cases (P < 0.00001) [Table 3]. IL-6 level has a significant association with SpO2 in COVID-19 pneumonia cases (P < 0.00001) [Table 4]. BIPAP/ NIV requirement during the course of COVID-19 pneumonia in critical care settings has a significant association with IL-6 level (P < 0.00001) [Table 5]. Timing of BIPAP/NIV requirement during the course of COVID-19 pneumonia in a critical care setting has a significant association with IL-6 level (P < 0.00001) [Table 6]. Follow-up IL-6 titer during hospitalization as compared to entry point abnormal IL-6 has a significant association in post-COVID lung fibrosis (P < 0.00001) [Table 7].
| HRCT severity | IL-6 level normal (n=990) | IL-6 level abnormal (n=1410) | Analysis |
|---|---|---|---|
| <8 score (n=500) | 391 | 109 | χ2=358.15 |
| 9–15 (n=800) | 236 | 564 | P<0.00001 |
| >15 (n=1100) | 363 | 737 |
HRCT: High-resolution computerized tomography, IL-6: Interleukin-6, COVID-19: Coronavirus disease-19
| Doi | IL-6 level normal (n=990) | IL-6 level abnormal (n=1410) | Analysis |
|---|---|---|---|
| <7 days (n=538) | 401 | 137 | χ2=400.72 |
| 8–15 days (n=951) | 209 | 742 | P<0.00001 |
| >15 days (n=911) | 338 | 573 |
IL-6: Interleukin-6, COVID-19: Coronavirus disease-19, Doi: Duration of illness
| Oxygen saturation | IL-6 level normal (n=990) | IL-6 level abnormal (n=1410) | Analysis |
|---|---|---|---|
| >90% (n=516) | 429 | 87 | χ2=583.05 |
| 75–90% (n=972) | 209 | 763 | P<0.00001 |
| <75% (n=912) | 274 | 638 |
IL-6: Interleukin-6, COVID-19: Coronavirus disease-19
| BIPAP/NIV | IL-6 level normal (n=990) | IL-6 level abnormal (n=1410) | Analysis |
|---|---|---|---|
| BIPAP/NIV required (n=1378) | 398 | 980 | χ2=204.24 |
| BIPAP/NIV not required (n=1022) | 592 | 430 | P<0.00001 |
BIPAP: Bi-level positive airway pressure, NIV: Non-invasive ventilation, IL-6: Interleukin-6, COVID-19: Coronavirus disease-19
| BIPAP used (n=1378) with duration of illness |
Abnormal IL-6 level (n=787) |
Four-fold raised IL-6 level (n=591) |
Analysis |
|---|---|---|---|
| Entry point <1 days (n=592) |
452 | 140 | χ2=157.05 P<0.00001 |
| 3–7 days (n=n= 432) | 181 | 251 | |
| After 7 days (n=354) | 154 | 200 |
BIPAP: Bi-level positive airway pressure, NIV: Non-invasive ventilation, IL-6: Interleukin-6, COVID-19: Coronavirus disease-19
| Post-COVID COVID pneumonia fibrosis | IL-6 titer increased/abnormal at entry point (n=690) | IL-6 titer fourfold increased during follow-up (n=720) | Analysis |
|---|---|---|---|
| Pulmonary fibrosis present (n=560) | 114 | 386 | χ2=211.78 |
| Pulmonary fibrosis absent (n=850) | 576 | 334 | P<0.00001 |
IL-6: Interleukin-6
Follow-up IL-6 titer during hospitalization as compared to entry point normal IL-6 has a significant association in post-COVID lung fibrosis (P < 0.00001) [Table 8]. Follow-up IL-6 titer during hospitalization as compared to entry point abnormal IL-6 has a significant association in predicting cytokine storm irrespective of normal or abnormal of IL-6 at entry point (P < 0.0001) [Table 9].
| Post-COVID COVID pneumonia fibrosis | IL-6 normal at entry point and remained less than fourfold (n=694) | IL-6 titer fourfold increased during follow-up (n=296) | Analysis |
|---|---|---|---|
| Pulmonary fibrosis present (n=191) | 29 | 162 | χ2=340.53 |
| Pulmonary fibrosis absent (n=799) | 665 | 134 | P<0.00001 |
IL-6: Interleukin-6
| Cytokine storm | Normal IL-6 titer at entry point (n=990) | Abnormal IL-6 at entry point (n=1410) | Analysis |
|---|---|---|---|
| Cytokine storm present (n=498) | 98 | 400 | χ2=120.65 |
| Cytokine storm absent (n=1902) | 892 | 1010 | P<0.00001 |
DISCUSSION
We have observed that computed tomography (CT) severity can be considered as the best visual marker of the severity of COVID-19 pneumonia which can be correlated with inflammatory markers such as IL-6, ferritin, CRP, LDH, D-dimer and lymphopenia, and lymphocyte-platelet ratio. In the present study, CT severity score at the entry point with D-dimer level has a significant correlation in COVID-19 pneumonia cases. [(P < p<0.00001]). COVID-19 cases with CT severity score <8, 8-–15 and >15 documented normal and abnormal IL-6 level in 391/109, 236/564, and 363/737, respectively of a total of 2400 study cases. Various authors[17-32] documented that IL-6 and other inflammatory markers such as CRP, ferritin, and LDH have been correlated with CT severity and cases from mild to moderate to severe were having increasing trends of inflammatory markers.
In the present study, IL-6 level has a significant association with Doi duration of illness in COVID-19 pneumonia cases. [(P < p<0.00001]). COVID-19 cases with Doi <7 days, 8-–15 days, and >15 days of onset of symptoms documented normal and abnormal IL-6 levels in 401/137, 209/742, and 338/573 cases, respectively. Rationale for the observation is not known; it may be that the inflammatory pattern is different during the first 1st and third 3rd weeks as compared to the second 2nd weeks of illness. We have also correlated IL-6 patterns with other inflammatory markers such as ferritin, CRP, and LDH and documented that these markers raised parallel to IL-6. Raised IL-6 after the second 2nd week illness may indicate worsening of COVID-19 pneumonia or secondary bacterial infection, which will guide the intensivist to screen for infection and formulate antibiotics policy accordingly. Thus, follow-up titers will guide indirectly in protocolized management in critical care settings.
In the present study, BIPAP/NIV requirement during the course of COVID-19 pneumonia in a critical care setting has a significant association with IL-6 level. [(P < p<0.00001]). COVID-19 cases received BIPAP/NIV during hospitalization were documented with normal and abnormal IL-6 levels in 398/980 and 592/430 cases, respectively. We have also documented that IL-6 level has a positive correlation with the requirement of BIPAP/NIV, high-flow nasal cannula (HFNC) oxygen supplementation, and invasive mechanical ventilation in critical care settings. Studies by various authors[21-39] have documented that high IL-6 is a predictor of critical illness requiring intensive care unit treatment, including non-invasive and invasive ventilatory support as compared to cases with normal IL-6 levels.
In the present study, IL-6 level has a significant association with SpO2 oxygen saturation in COVID-19 pneumonia cases. [(P < p<0.00001]). COVID-19 cases with SpO2 oxygen saturation >90%, 75-–90%, and <75% were observed as normal and abnormal IL-6 levels in 429/87, 209/763, and 274/638 cases, respectively. We have also documented that hypoxia at the entry point during hospitalization has a positive correlation with abnormal IL-6 levels. Numerous authors[23-37] have documented that a higher IL-6 level is associated with hypoxemia, also mentioned that higher IL-6 level is an indicator of an advanced pneumonia process and progressed lung parenchymal inflammatory injury or necrosis resulting in failure of oxygenation.
In the present study, timing of BIPAP/NIV requirements during the course of COVID-19 pneumonia in a critical care setting has a significant association with IL-6 level. [(P < p<0.00001]). COVID-19 cases received BIPAP/ NIV at entry point <1 day, 3-–7 days, and after 7 days of hospitalization were documented significance in four-fold raised IL-6 levels in 452/140, 181/251, and 154/200 cases, respectively. We have also observed that early initiation of BIPAP/NIV in COVID-19 pneumonia cases meeting the criteria of oxygen supplementation, that is, SpO2 oxygen saturation <89% at room air during hospitalization were having a beneficial effect in controlling systemic immune inflammatory syndrome, which can be measured by IL-6 level in follow-up. Rationality for similar observations may be due to improvement in oxygenation and lung compliance after the use of BIPAP/NIV in these cases. The plausible mechanism is that hypoxia is an important trigger for the rise in inflammatory markers by means of a rise in hypoxia inducible transcription factors. Previously published studies by various authors[37-41] have documented similar observations to our study and noted higher levels of IL-6 titer in those cases that required ventilatory support during hospitalization in intensive care units.
In the present study, we have observed that entry point normal and abnormal IL-6 titer has a significant association with cytokine storm [(P < p<0.00001]). Total COVID-19 cases with cytokine storm (498/2400) have normal 98/498 and abnormal 400/498 IL-6 titer. Total COVID-19 cases without cytokine storm (1902/2400) have 892/1902 and 1010/1902 have entry point abnormal IL-6 titer. We have also documented that ‘Cytokine storm’ is an independent predictor of poor outcome, and many of these cases represent rapidly evolving COVID-19 pneumonia progressing to ARDS and requiring ventilatory support. We have followed all these cases with cytokine storm and observed that a proportionately large number of these cases were required high-flow oxygen supplementation for a longer duration during hospitalization, and a few cases required oxygen supplementation at home for 3 months after discharge from the critical care setting. Numerous authors[18-31] have documented similar observations to our study. We have documented the significant role of tocilizumab in curtailing ‘cytokine storm’ with severe COVID-19 pneumonia cases requiring ventilatory support, and it will show improvement in oxygenation, inflammatory markers titer, ventilatory support requirement in the majority of cases, and mortality benefit in few cases. Thus, timely IL-6 inhibitor or tocilizumab has outcome a modifying role in intensive care units in cases with acute lung injury (ALI)/ ARDS with IL-6 level above 100 pg/mL. Various authors[31-46] have documented similar to our findings in their studies and mentioned that IL-6 targeted treatment will help in disease progression and good treatment outcomes.
In the present study, radiological outcome as post-COVID lung fibrosis has a significant association with a fourfold rise in follow-up IL-6 titer during hospitalization in cases with abnormal IL-6 titer at the entry point. (P < 0.00001). In post-COVID-19 lung fibrosis cases with abnormal IL-6 (560/1410) at the entry point, 114/560 and 386/560 cases had abnormal and four-fold rises in IL-6 titer, respectively. In COVID-19 cases without radiological sequel (850/1410) and abnormal IL-6 at the entry point, 576/850 and 334/850 cases had an abnormal and four-fold rises in IL-6 titer, respectively. We have also documented that serial measurement of IL-6 during hospitalization irrespective of the entry point abnormal level has very well correlation with the requirement of interventions in indoor and intensive care units such as high flow nasal cannula (HFNC), BIPAP/NIV (bilevel positive airway pressure/Noninvasive ventilation), and invasive mechanical ventilation. Cases with cytokine storm were picked up earlier by serial IL-6 level, and a proportionately large number will have post-COVID lung fibrosis. Thus, IL-6 will indirectly help in predicting the future risk of the development of post-COVID lung fibrosis. Authors[34-42] have observed similar findings in their respective studies and reported rising titers of IL-6 which is a marker of exaggerated lung inflammation and necrosis, which will result in lung fibrosis.
In the present study, radiological outcome as post-COVID lung fibrosis has a significant association with four-fold rise in follow-up IL-6 titer during hospitalization in cases with normal or less than four-fold IL-6 titer at the entry point. (P < 0.00001). In post-COVID-19 lung fibrosis cases with abnormal IL-6 (191/990) at the entry point, 29/191 and 162/191 cases had normal or less than four-fold IL-6 titer at the entry point and a sequential four-fold rise in IL-6 titer, respectively. In COVID-19 cases without radiological sequel (799/990) and abnormal IL-6 at the entry point, 665/799 and 134/799 cases had normal or less than four-fold IL-6 titer at the entry point and a serial four-fold rise in IL-6 titer, respectively. We have also documented that normal IL-6 is a predictor of good clinical and radiological outcomes, and serial measurement of IL-6 during hospitalization, irrespective of entry point level, has a very good correlation with underlying lung pathology. We have observed that IL-6 rising trends would help in predicting exaggerated underlying lung parenchymal damage secondary to cytokine induced lung necrosis and cytokine induced ALI (Acute lung injury)/ARDS (acute respiratory distress syndrome). These insults such as necrosis or ALI/ARDS are considered as early markers of future lung fibrosis. Authors[23-31, 37-46] documented similar observations and mentioned the importance of serial IL-6 titers in assessing high-risk cases for respiratory failure. They have observed the role of follow-up IL-6 titers in assessing critical COVD-19 cases and the crucial role in de-escalating interventions in the intensive care units along with clinical assessment. Authors have documented rising trends of IL-6 as a marker of post-COVID lung fibrosis.
We have documented that the age and gender of included cases have a significant association with IL-6 level. Studies by various authors[23-31,37-46] also documented similar observations. In the present study, comorbidity as diabetes mellitus, COPD, hypertension, IHD, and obesity has significant association IL-6 level [(P < p<0.00001].). Studies by various authors[23-31,37-46] also documented similar observations in IL-6 level and its correlation with underlying comorbidities.
Limitations of study
We have studied all important aspects of IL-6 in COVID-19 pneumonia from entry points in indoor units till 12 weeks of discharge with an adequate sample size. Still, we have documented a few limitations in our study.
The first limitation is that we have excluded cases that expired during the study period and those not willing to follow-up. Thus, the exact role of analyzing disease severity and predicting mortality in pour study cases was not done.
The second limitation is that, the effect of the confounding factors, such as other inflammatory conditions causing abnormal IL-6 titer such as infective, inflammatory, and rheumatological disorders, were not done during the entire duration of 12 weeks and its effect on COVID-19 severity parameters was not possible.
The third limitation is that the association of IL-6 titer with the requirement of other modes of intensive care treatments, such as high-flow nasal cannula and invasive mechanical ventilatory support, is not assessed differently. Our clinical intrusion is that the cases predominantly on BIPAP/NIV were considered as ventilatory support, probably because the majority of COVID-19 cases receiving high-flow nasal cannula were shifted to BIPAP/NIV and or mechanical ventilation in intensive care units.
Implications to clinical practice and implications to future research
The role of IL-6 in COVID-19 pandemic has been studied widely during all three waves with variants such as Wuhan, delta, and omicron. In each wave, IL-6 has a documented role in predicting severity, course during hospitalization, guided interventions requirement in indoor settings, and helped in analyzing the final outcomes. The role of sequential IL-6 titers in predicting deadly cytokine storms has been evaluated globally, and IL-6-guided therapy has documented effects on outcomes in COVID-19 pneumonia. We recommend further evaluation and more global research-
Although cytokine storms have been documented in rheumatological conditions, which is similar to COVID-19 pneumonia, the outcome and response to therapy is different.
Cytokine storm was common in all variants of COVID-19, but presentation was different and manifested as pulmonary type in the delta variant, pulmonary plus extrapulmonary om Wuhan variant, and predominant extrapulmonary type in the omicron variant. Rationale for these findings mandates more workup.
Cytokine storm and IL-6 surge were documented, which are selected cases of COVID-19. IL-6 titer required for labeling cytokine storms is validated. Discordance between IL-6 titer and cytokine storm has been documented in all three waves of COVID-19. Many patients with less than a four-fold rise in titer were having cytokine storm-like presentations, while few cases with more than 16-fold rise in titer were not having symptoms of the cytokine storm. Rationale for similar observations need more research.
Rationale for a disproportionate surge of IL-6 as per the genetic makeup of the virus is an issue of real research.
Finally, patients’ characteristics or high-risk indicators for cytokine storm or IL-6 surge need further research.
CONCLUSION
IL-6 is an easily available and sensitive marker of inflammation and has a documented ‘“game changer’ changer” role in COVID-19 pneumonia. IL-6 titer assessment at the entry point has documented a crucial role in the initial assessment of the severity of COVID-19 illness and guided in triaging the case to admission in different utilities from the indoor unit to the critical care unit. Thus, IL-6 titer has been observed to play an important role in predicting the need for ventilatory support and also guided positive outcomes through early use of these interventions in critical care units. IL-6 titer at the entry point has indirectly helped in predicting the final outcome because the majority of patients presenting with normal or abnormal titers have behaved differently and, in these scenarios, sequential titers have played a crucial role. IL-6 follow titer analysis has shown a significant impact in predicting real time course during hospitalization than entry point titer. Sequential IL-6 titer has also guided the exact risk of ‘cytokine storm’ than entry point titer as the majority of entry point normal titer has progressed to advanced disease in a short time, and these cases were easily picked up by easily available follow titer. Sequential titer is the best predictor of final radiological outcome as the majority of cases with increased follow-up titers were having post-COVID lung fibrosis than entry point normal IL-6 titer. Thus, we recommend follow-up titer assessment in all cases to have a successful treatment outcome by means of timely honoring these cases with interventions and preventing poor clinical and radiological outcomes.
Ethical approval
Approved by the IRB/IEC at Venkatesh Hospital and Critical Care Center Latur India and MIMSR Medical College Latur India, number VCC/119-2020-2021, dated 22/11/2020.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Characteristics of SARS-CoV-2 and COVID-19. Nat Rev Microbiol. 2021;19:141-54.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet. 2020;395:1054-62.
- [CrossRef] [PubMed] [Google Scholar]
- Dysregulation of immune response in patients with Coronavirus 2019 (COVID-19) in Wuhan, China. Clin Infect Dis. 2020;71:762-8.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical features of 69 cases with Coronavirus disease 2019 in Wuhan, China. Clin Infect Dis. 2020;71:769-77.
- [CrossRef] [PubMed] [Google Scholar]
- Role of initial and follow-up IL-6 (interleukin-6) titre in COVID-19 pneumonia: A single center experience. Electron J Gen Med. 2022;19:Em390.
- [CrossRef] [Google Scholar]
- Role of interleukin-6 in Coronavirus disease 2019 pneumonia: Sensitive marker of inflammation, a predictor of ventilatory support and early marker of post-Coronavirus disease lung fibrosis. A single center experience. Egypt J Chest Dis Tuberc. 2023;72:346-54.
- [CrossRef] [Google Scholar]
- Serial interleukin-6 titer monitoring in COVID-19 pneumonia: Valuable inflammatory marker in the assessment of severity, predicting ventilatory support requirement, and final radiological outcome-prospective observational study in tertiary care setting in India. J Assoc Pulmonologist Tamil Nadu. 2022;5:2-8.
- [CrossRef] [Google Scholar]
- The role of initial and follow-up C-reactive protein titer in COVID-19 pneumonia: A single-center study of 1000 cases in a tertiary care setting in India. J Adv Lung Health. 2023;3:17-24.
- [CrossRef] [Google Scholar]
- Serial CRP (C-reactive protein) monitoring in COVID-19 pneumonia for the assessment of severity, ventilatory support requirement and predicting early lung fibrosis. J Med. 2022;23:112-20.
- [CrossRef] [Google Scholar]
- Role of initial and follow-up LDH titer in COVID-19 pneumonia: A single center experience of 2000 cases in tertiary care setting in India. J Med. 2023;24:10-7.
- [CrossRef] [Google Scholar]
- Role of initial and follow-up lactate dehydrogenase titer in Coronavirus disease 2019 pneumonia: A single-center experience. CHRISMED J Health Res. 2023;10:79-85.
- [CrossRef] [Google Scholar]
- Role of ferritin as “core marker” in the assessment of severity, response to therapy and predicting outcome in COVID-19 pneumonia: A large, two-center, prospective, observational study of 1000 cases in tertiary care setting in India. Indian J Respir Care. 2022;11:253-60.
- [CrossRef] [Google Scholar]
- Role of “Ferritin” in COVID-19 pneumonia: Sensitive marker of inflammation, predictor of mechanical ventilation, and early marker of post COVID-lung fibrosis-a prospective, observational, and interventional study in a tertiary care setting in India. Muller J Med Sci Res. 2022;13:28-34.
- [CrossRef] [Google Scholar]
- "Serial ferritin titer" monitoring in COVID-19 pneumonia: Valuable inflammatory marker in assessment of severity and predicting early lung fibrosis-prospective, multicentric, observational, and interventional study in tertiary care setting in India. Egypt J Intern Med. 2022;34:75.
- [CrossRef] [PubMed] [Google Scholar]
- Role of D-Dimer in assessing severity, monitoring, and predicating outcome in COVID-19 pneumonia: A single center study. Glob J Health Sci Res. 2023;1:31-7.
- [CrossRef] [Google Scholar]
- CO-RADS: A categorical CT assessment scheme for patients suspected of having COVID-19-definition and evaluation. Radiology. 2020;296:E97-104.
- [CrossRef] [PubMed] [Google Scholar]
- Performance of the Roche IL-6 chemiluminescent immunoassay in patients with COVID-like respiratory symptoms. J Virol Methods. 2021;296:114224.
- [CrossRef] [PubMed] [Google Scholar]
- Serum interleukin-6 is an indicator for severity in 901 patients with SARS-CoV-2 infection: A cohort study. J Transl Med. 2020;18:406.
- [CrossRef] [PubMed] [Google Scholar]
- Association between cytokine profiles and lung injury in COVID-19 pneumonia. Respir Res. 2020;21:201.
- [CrossRef] [PubMed] [Google Scholar]
- Into the eye of the cytokine storm. Microbiol Mol Biol Rev. 2012;76:16-32.
- [CrossRef] [PubMed] [Google Scholar]
- Cytokine storm intervention in the early stages of COVID-19 pneumonia. Cytokine Growth Factor Rev. 2020;53:38-42.
- [CrossRef] [PubMed] [Google Scholar]
- An interferon-gamma-related cytokine storm in SARS patients. J Med Virol. 2005;75:185-94.
- [CrossRef] [PubMed] [Google Scholar]
- Pathogenic human Coronavirus infections: Causes and consequences of cytokine storm and immunopathology. Semin Immunopathol. 2017;39:529-39.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical progression and cytokine profiles of middle east respiratory syndrome Coronavirus infection. J Korean Med Sci. 2016;31:1717-25.
- [CrossRef] [PubMed] [Google Scholar]
- Plasma inflammatory cytokines and chemokines in severe acute respiratory syndrome. Clin Exp Immunol. 2004;136:95-103.
- [CrossRef] [PubMed] [Google Scholar]
- Using IL-2R/ lymphocytes for predicting the clinical progression of patients with COVID-19. Clin Exp Immunol. 2020;201:76-84.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of interleukin-6 and its association with the severity of disease in COVID-19 patients. Indian J Med Spec. 2020;11:132-6.
- [CrossRef] [Google Scholar]
- Could IL-6 predict the clinical severity of COVID-19? Turk J Biochem. 2021;46:499-507.
- [CrossRef] [Google Scholar]
- Effective treatment of severe COVID-19 patients with tocilizumab. Proc Natl Acad Sci U S A. 2020;117:10970-5.
- [CrossRef] [PubMed] [Google Scholar]
- Biomarker variation in patients successfully treated with tocilizumab for severe Coronavirus disease 2019 (COVID-19): Results of a multidisciplinary collaboration. Clin Exp Rheumatol. 2020;38:742-7.
- [Google Scholar]
- Outcomes and biomarker analyses among patients with COVID-19 treated with interleukin 6 (IL-6) receptor antagonist sarilumab at a single institution in Italy. J Immunother Cancer. 2020;8:e001089.
- [CrossRef] [PubMed] [Google Scholar]
- The correlation between viral clearance and biochemical outcomes of 94 COVID-19 infected discharged patients. Inflamm Res. 2020;69:599-606.
- [CrossRef] [PubMed] [Google Scholar]
- Longitudinal changes of inflammatory parameters and their correlation with disease severity and outcomes in patients with COVID-19 from Wuhan, China. Crit Care. 2020;24:525.
- [CrossRef] [PubMed] [Google Scholar]
- IL-6: Relevance for immunopathology of SARS-CoV-2. Cytokine Growth Factor Rev. 2020;53:13-24.
- [CrossRef] [PubMed] [Google Scholar]
- interleukin-6 is a biomarker for the development of fatal severe acute respiratory syndrome Coronavirus 2 pneumonia. Front Immunol. 2021;12:613422.
- [CrossRef] [PubMed] [Google Scholar]
- Weathering the cytokine storm in COVID-19: Therapeutic implications. Cardiorenal Med. 2020;10:277-87.
- [CrossRef] [PubMed] [Google Scholar]
- Profiling serum cytokines in COVID-19 patients reveals IL-6 and IL-10 are disease severity predictors. Emerg Microbes Infect. 2020;9:1123-30.
- [CrossRef] [PubMed] [Google Scholar]
- IL-6-based mortality risk model for hospitalized patients with COVID-19. J Allergy Clin Immunol. 2020;146:799-807.
- [CrossRef] [PubMed] [Google Scholar]
- Elevated levels of IL-6 and CRP predict the need for mechanical ventilation in COVID-19. J Allergy Clin Immunol. 2020;146:128-36.e4.
- [CrossRef] [PubMed] [Google Scholar]
- Elevated interleukin-6 and severe COVID-19: A meta-analysis. J Med Virol. 2020;92:2283-5.
- [CrossRef] [PubMed] [Google Scholar]
- Interleukin-6 as prognosticator in patients with COVID-19. J Infect. 2020;81:452-82.
- [CrossRef] [PubMed] [Google Scholar]
- Tocilizumab in patients with severe COVID-19: A retrospective cohort study. Lancet Rheumatol. 2020;2:e474-84.
- [CrossRef] [PubMed] [Google Scholar]
- IL-6 inhibitors in the treatment of serious COVID-19: A promising therapy? Pharmaceut Med. 2020;34:223-31.
- [CrossRef] [PubMed] [Google Scholar]
- Prognostic value of interleukin-6, C-reactive protein, and procalcitonin in patients with COVID-19. J Clin Virol. 2020;127:104370.
- [CrossRef] [PubMed] [Google Scholar]
- Detectable serum severe acute respiratory syndrome Coronavirus 2 viral load (RNAemia) is closely correlated with drastically elevated interleukin 6 level in critically ill patients with Coronavirus disease 2019. Clin Infect Dis. 2020;71:1937-42.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic utility of clinical laboratory data determinations for patients with the severe COVID-19. J Med Virol. 2020;92:791-6.
- [CrossRef] [PubMed] [Google Scholar]