Translate this page into:
Subcutaneous extraskeletal osteosarcoma of the foot: A case report
*Corresponding author: Leena Dennis Joseph, Department of Pathology, Sri Ramachandra Institute of Higher Education and Research, Chennai, Tamil Nadu, India. leenadennisj@sriramachandra.edu.in
-
Received: ,
Accepted: ,
How to cite this article: Sneha K, Joseph LD, Susruthan M, Ramya R. Subcutaneous extraskeletal osteosarcoma of the foot: A case report. Sri Ramachandra J Health Sci 2021;1:25-7.
Abstract
Extraskeletal osteosarcoma (ESOS) is a rare variant of osteosarcoma which occurs exclusively in the soft tissue without any bone involvement. Subcutaneous ESOS, in particular, is very rare and is seen in <10% of cases. Here, we report a case of a subcutaneous tumor in the fourth web space of the left foot in a 73-year-old man. The diagnosis of ESOS was made on histology and by immunohistochemical reactivity to special AT-rich sequence-binding protein 2 (SATB2), which is a sensitive, nuclear marker of osteoblastic differentiation. We present this case because of its rarity and the use of SATB2 immunohistochemistry to confirm the diagnosis.
Keywords
Osteosarcoma
Extraskeletal
Subcutaneous
Special AT-rich sequence-binding protein 2
INTRODUCTION
Extraskeletal osteosarcoma (ESOS) is a rare soft-tissue tumor, accounting for only 1% of all soft-tissue sarcomas and 2–4% of all osteosarcomas.[1,2] Most often ESOS is located in the deep soft tissues of the extremities. ESOS occurring in the subcutaneous tissue is extremely rare, seen in <10% of the cases.[3] A small percentage of cases have an association with the previous radiotherapy or trauma.[4] The prognosis is usually poor but the overall survival rates are higher as compared to skeletal osteosarcoma.[5] Special AT-rich sequence-binding protein 2 (SATB2) is a sensitive marker for osteoblastic lineage and is positive in malignant bone and soft-tissue tumors with osteoblastic differentiation or bone formation.[6]
In this report, we present a case of subcutaneous ESOS of the dorsum of the left foot, focusing on the clinicopathological features, and immunohistochemical reactivity to SATB2 and prognosis.
CASE REPORT
A 73-year-old man presented to the surgery clinic with a swelling over the left foot for 1 month. The swelling had progressively increased in size with recent onset of pain at the site since a week. No history of trauma or therapy was reported. His physical examination revealed a round, firm, and solid mass measuring 3.5 × 3.2 × 3.1 cm located in the fourth web space of the dorsum the left foot. External surface was smooth with well-defined margins and restricted mobility.
Radiograph of the dorsum of the left foot showed a soft-tissue mass with specks of calcification. Magnetic resonance imaging (MRI) of the left foot revealed a heterogeneous, well circumscribed soft-tissue lesion with specks of calcification. There was no involvement of the adjacent bones and joint. The radiological diagnosis was that of an infected cyst or hematoma [Figure 1a].
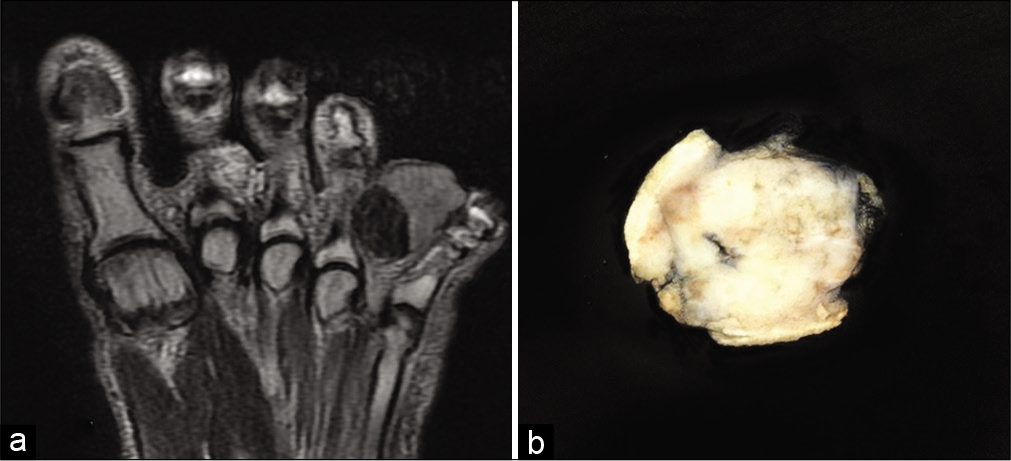
- (a) A grey white, homogeneous, fairly circumscribed lesion is seen underlying the skin measuring 3.2 × 3.1 × 2.5 cm. (b) Magnetic resonance imaging of foot- soft-tissue lesion measuring 35 × 31 × 32 mm is seen at the fourth interphalangeal region.
Macroscopic examination revealed a skin covered soft-tissue mass measuring 3.2 × 3.1 × 2.5 cm. Cut surface showed a nodular mass which was gray white, homogenous with hard and gritty areas [Figure 1b]. Microscopy showed skin with a focus of ulceration and underlying tumor tissue composed of neoplastic cells arranged in sheets and trabeculae [Figure 2]. The tumors are pleomorphic, round to polygonal with scant eosinophilic cytoplasm and hyperchromatic nuclei. Abundant osteoid matrix rimmed by the pleomorphic tumor cells was also noted [Figure 3a and b]. Mitotic activity was noted up to 12 per ten high power fields.
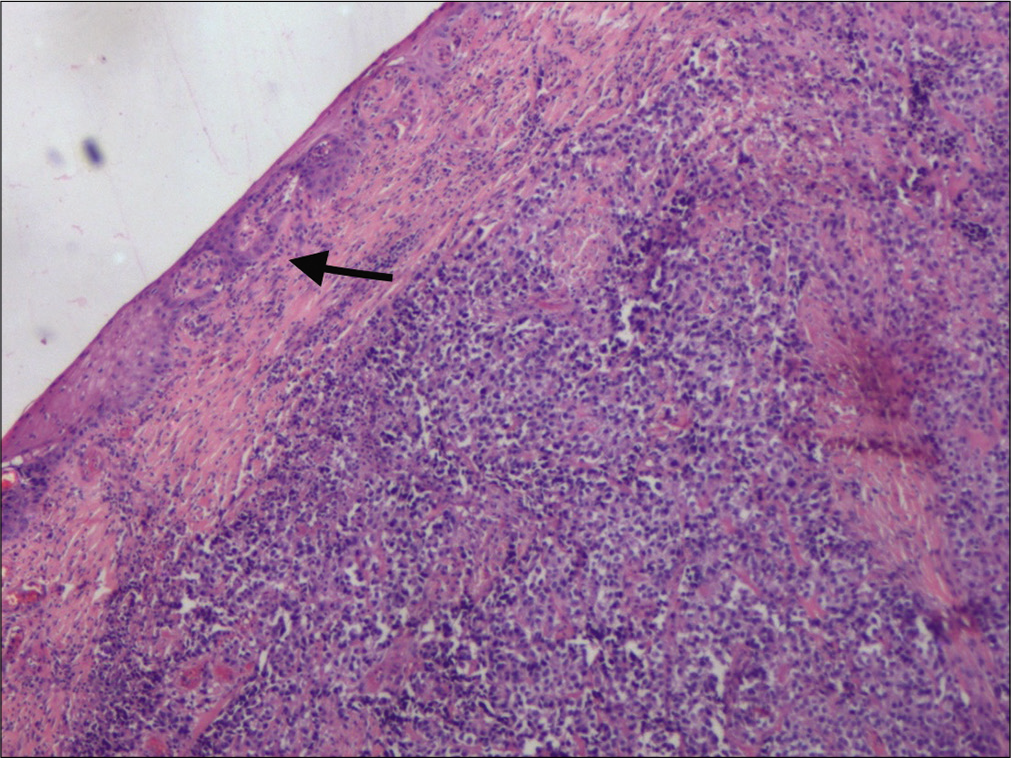
- Thinned out skin (arrow) with an underlying ill circumscribed lesion. Hematoxylin and eosin ×40.
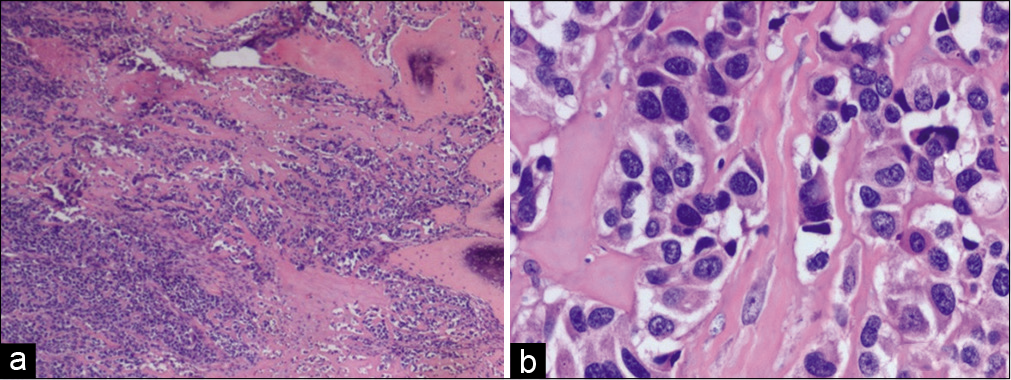
- (a) Tumor cells with osteoid and focal bone formation (arrow). Hematoxylin and eosin (H and E) ×40. (b) Polygonal pleomorphic tumor cells with areas of osteoid deposition. H and E ×400.
Immunohistochemical staining was positive for Vimentin and SATB2. SATB2 is a novel, sensitive nuclear marker for osteoblastic differentiation [Figure 4]. Ki67 labeling index was 30%. Focal positivity for S100 was also seen. Stains for p63, SMA, HMB45, and cytokeratin were negative which helped in eliminating the differential diagnosis of clear cell sarcoma, malignant peripheral nerve sheath tumor with heterologous elements, dedifferentiated liposarcoma, and poorly differentiated carcinoma. The above-mentioned findings led to the conclusion that this subcutaneous tumor was an ESOS.
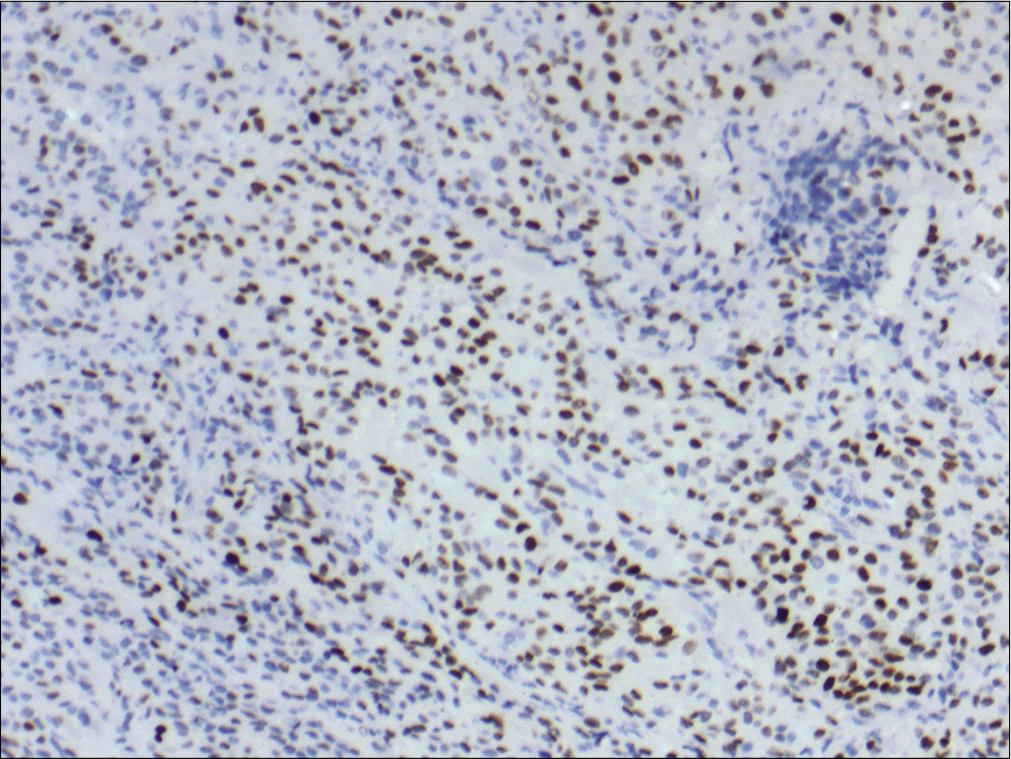
- Special AT-rich sequence-binding protein 2 nuclear positivity in the tumor cells. Immunohistochemistry ×100.
DISCUSSION
ESOS was first described in 1941 by Wilson and is defined as a malignant neoplasm composed of cells producing osteoid, devoid of attachment to the bone or periosteum.[7,8] Unlike osteosarcomas of bone, ESOSs are encountered in patients after the age of 40 years.[7,9] Most tumors arise in the deep soft tissues of extremities but occasional lesions can be confined to the subcutis or even the dermis.
Only a very few cases of primary ESOS with subcutaneous location have been reported.[10] Tamura et al. identified 18 cases of primary subcutaneous ESOS after performing a PubMed search. In the study, 30% of the cases were aged below 40 years. Subcutaneous ESOS may develop at a younger age as compared to deep seated ESOS. Subcutaneous ESOS is usually <5 cm in size.[3] In a large case study of ESOS (n = 266), the median size was 10 cm with 80% of cases being >5 cm in size.[11] Usually, it is considered that ESOS is >5 cm in size. Although majority of ESOS are reported in the extremities, subcutaneous ESOS can occur in non-extremities such as trunk, scalp, and abdominal wall.[3]
Radiological assessment of ESOS is best performed by computed tomography (CT) and MRI. On CT, the lesion typically has central calcification, but its absence does not exclude the diagnosis. MRI studies show a mass that is hypointense on T1-weighted images and hyperintense on T2-weighted images.[5]
Histology of ESOS is similar to osteosarcomas of bone and ESOS can contain a wide range of histologic patterns with differing amounts of osteoid, cartilaginous, and fibrous tissues. The osteoid is usually deposited in a lace-like or trabecular pattern and occasionally as mature appearing bone. Majority of the cases have the picture of an undifferentiated pleomorphic sarcoma. The chondroblastic variant contains atypical cartilage with focal bone formation. Giant cell variant of ESOS is associated with the presence of benign and malignant multinucleated osteoclastic giant cells.[8,12]
SATB2 is a novel and sensitive nuclear marker for osteoblastic differentiation. SATB2 is an essential nuclear factor in the osteoblastic cell lineage. In the study by Conner and Hornick, all cases of conventional bone osteosarcoma (n = 53), 89% cases (n = 9) of ESOS were positive for SATB2. Other malignant tumors of bone and soft-tissue showed immunoreactivity to SATB2 which was primarily limited to areas of heterologous differentiation.[6]
The overall survival of ESOS is poor, ranging from 25% to 75% at 5 years. Poor prognostic factors include large tumor size, incomplete resection, and metastatic disease. However, the survival rates of subcutaneous ESOS are comparably better than deep seated ESOS. It may be due to the superficial nature of the lesion resulting in earlier diagnosis and prompt treatment.[5]
The primary treatment of ESOS involves surgical resection with wide resection margins. Adjuvant radiation and chemotherapy may also be incorporated to decrease the risk of recurrence.[5]
CONCLUSION
ESOS is a rare malignant soft-tissue tumor, even more so in the subcutaneous location which can be diagnostically challenging. The histomorphology and radiology can aid in the diagnosis. In doubtful cases, immunohistochemistry with SATB2 can clinch the diagnosis.
Acknowledgments
None.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Diagnostic imaging of benign and malignant osseous tumors of the fingers. Radiographics. 2014;34:1954-67.
- [CrossRef] [PubMed] [Google Scholar]
- Extraskeletal osteosarcoma arising in the subcutaneous tissue of the lower leg: A case report and literature review. Mol Clin Oncol. 2018;9:287-92.
- [CrossRef] [PubMed] [Google Scholar]
- Subcutaneous extraskeletal osteosarcoma of the forearm: A case report and review of the literature. Skeletal Radiol. 2016;45:1307-11.
- [CrossRef] [PubMed] [Google Scholar]
- SATB2 is a novel marker of osteoblastic differentiation in bone and soft tissue tumours. Histopathology. 2013;63:36-49.
- [CrossRef] [PubMed] [Google Scholar]
- Extraskeletal subcutaneous osteosarcoma of the upper arm: A case report. Oncol Lett. 2011;2:75-7.
- [CrossRef] [PubMed] [Google Scholar]
- Osteogenic sarcoma of the somatic soft tissues. Clinicopathologic study of 26 cases and review of literature. Cancer. 1971;27:1121-33.
- [CrossRef] [Google Scholar]
- Extraskeletal osteosarcoma in Japan: Multiinstitutional study of 20 patients from the Japanese musculoskeletal oncology group. J Orthop Sci. 2007;12:424-9.
- [CrossRef] [PubMed] [Google Scholar]
- Postradiation soft tissue sarcomas: An analysis of 53 cases. Cancer. 1988;62:2330-40.
- [CrossRef] [Google Scholar]
- Extraskeletal osteosarcoma: A European musculoskeletal oncology society study on 266 patients. Eur J Cancer. 2017;74:9-16.
- [CrossRef] [PubMed] [Google Scholar]
- Extraskeletal osteosarcoma-a case report. J Clin Diagn Res. 2016;10:ED03-4.
- [CrossRef] [PubMed] [Google Scholar]






