Translate this page into:
Expect the unexpected – sinonasal papillary intestinal adenocarcinoma – A case report
*Corresponding author: V. Pavithra, Department of Pathology, Sri Ramachandra Medical College, Chennai, Tamil Nadu, India. pavithrav@sriramachandra.edu.in
-
Received: ,
Accepted: ,
How to cite this article: Anusuya C, Pavithra V, Kumar P, Rajendiran S. Expect the unexpected – sinonasal papillary intestinal adenocarcinoma – A case report. Sri Ramachandra J Health Sci 2022;2:33-5.
Abstract
Intestinal-type adenocarcinoma (ITAC) is the second most frequent sinonasal adenocarcinoma. High incidence of these tumors was seen among workers with occupational wood dust exposure, particularly of hardwood dusts. Furthermore, ITACs associated with dust exposure were diagnosed mostly in men (85–95%) and predominantly in the ethmoid sinus. This contrasts with sporadic ITACs that are more frequent in women and often arise in the maxillary antrum. ITAC had striking histomorphologic and immunophenotypic similarities with colorectal adenocarcinomas, but on the level of molecular pathologic mechanisms, these tumors have their own specific features different from gastrointestinal tumors. A 58-year-old female came with the chief complaints of difficulty in breathing and left-sided nasal obstruction for the past 1 month. On local examination, nasal septum was deviated to the right side on visualizing the left nasal cavity showed a polypoidal growth occupying the entire nasal cavity. Paranasal sinuses with contrast computed tomography (CT) showed a chronic granulomatous lesion in the left nasal cavity with surrounding inflammatory changes involving the ipsilateral sinuses. This patient was planned for functional endoscopic sinus surgery and specimen was sent for histopathological diagnosis. Contradictory to CT scan result, on gross and histopathology, the lesion was diagnosed to be intestinal type of sinonasal adenocarcinoma.
Keywords
Sinonasal
Intestinal adenocarcinoma
Papillary
INTRODUCTION
Intestinal-type adenocarcinoma (ITAC) is the second most common type of sinonasal adenocarcinoma after adenoid cystic carcinoma. It is composed of subtypes as described by Dr. Barnes that resemble carcinomas or adenomas of intestinal origin and occasionally the normal intestinal mucosa. ITACs occur mostly in males with a wide age range and a mean of 50–64 years. ITACs are most frequently localized in the ethmoid sinus (40%), the nasal cavity (25%), and the maxillary antrum (20%). Rare tumors with intestinal-type differentiation may also occur in other areas of the upper airways and in lung. ITACs are aggressive malignancies with frequent local spread to the orbit, the skull base, and the intracranial space, and with a possibility of metastatic spread.
CASE REPORT
A middle aged female came to our hospital with the chief complaint of difficulty in breathing along with the left nasal obstruction for the past 1 month. On local examination, nasal septum was deviated to the right side on visualizing the left nasal cavity showed a polypoidal growth occupying the entire nasal cavity at the level of anterior and the inferior turbinates.
Radiological examination of contrast computed tomography (CT) of paranasal sinuses revealed to be a chronic granulomatous lesion in the left nasal cavity with surrounding inflammatory changes involving the ipsilateral sinuses causing blockage of the left OMU complex and frontal sinus drainage pathway [Figure 1].
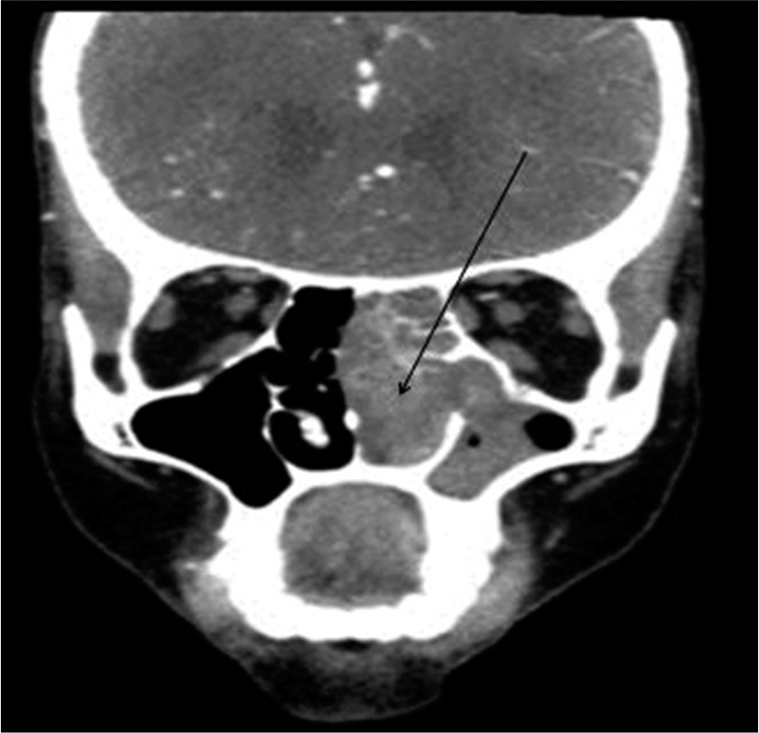
- Contrast computed tomography of paranasal sinuses: Lesion in the left nasal cavity (arrow).
The patient underwent endoscopic sinus surgery and a large soft-tissue density lesion of approximate size 5.8 × 1.8 × 3.3 cm (AP × TRANS × CC) which was occupying the entire nasal cavity was excised and sent for histopathological examination.
On microscopy, it was diagnosed to be intestinal type of papillary sinonasal adenocarcinoma predominantly showing a papillary growth pattern with tubular elements [Figure 2] composed of cuboidal to columnar epithelial cells having palisaded hyperchromatic nuclei and a few goblet cells [Figure 3]. Increased atypical mitotic activity and necrosis [Figure 4] were also seen.
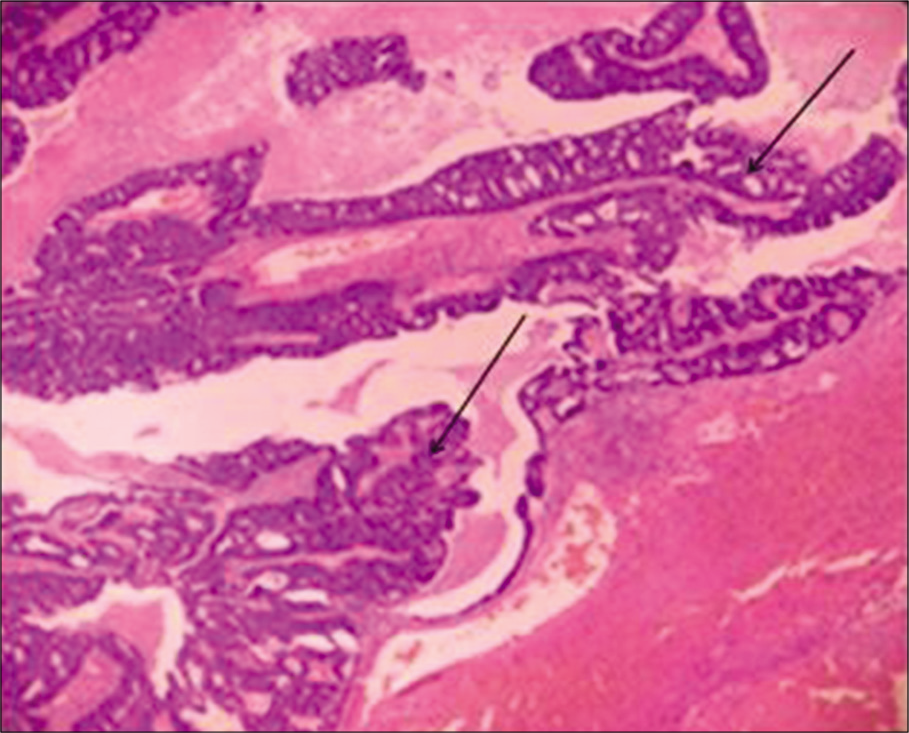
- H&E: Intestinal (arrow) type of papillary sinonasal adenocarcinoma ×40.
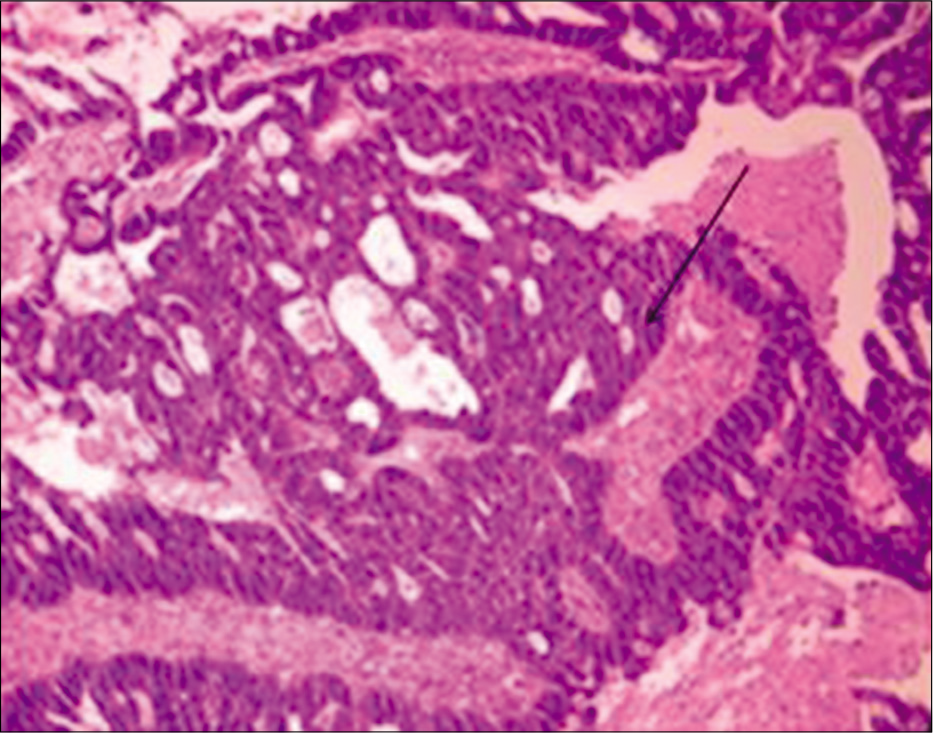
- H&E: Palisaded hyperchromatic nuclei (arrow) and a few goblet cells × 200.

- H&E: Necrosis (arrow) ×200.
DISCUSSION
ITAC mimics the appearance of the mucosa of the normal and neoplastic large and small intestine. The gross appearance of these tumors is similar to that of colonic adenocarcinoma.[1] In the Barnes classification, papillary subtype of ITAC (18% of all) shows prominent papillary fronds with minor amounts of tubular structures.[2] ITACs of this type usually contain columnar goblet cells and they often resemble intestinal villous or tubular adenomas. Rarely, papillary ITACs may recapitulate the morphology of the normal intestinal mucosa with nearly normal looking villi including the specialized cell types (goblet, resorptive, Paneth, and argentaffin cells) and the muscularis mucosae. The behavior of ITAC is that of high-grade malignancy showing recurrences, cervical lymph node metastasis, and distant metastasis, especially well-differentiated papillary type will have indolent course. It has been suggested that the papillary ITAC may have the best prognosis, as it typically behaves as a smoldering, locally destructive lesion with a limited tendency for regional or distant metastases.[3] The main differential diagnosis includes metastasis from colonic adenocarcinoma which is rare but most important differential. If in case, there is a trouble to differentiate from the metastasis immunohistochemistry which is usually CEA+, CK7-, and chromogranin-[4] can be used for the diagnostic purpose. The clinical features and colonoscopy can also play a major role in differentiating.[5] The treatment of ITAC is surgical resection varying from lateral rhinotomy to partial maxillectomy and total maxillectomy, with or without radiotherapy.
CONCLUSION
Sinonasal ITACs have a unique phenotype. The distinction between ITAC and non-ITAC is critical, as the two neoplasms have different clinical behavior and prognosis.[6] In our case, the histology played a key role in guiding treatment and it is very important that biopsy is accurately obtained and the slides are analyzed by a pathologist with specific expertise. In fact, the rarity of sinonasal tumors and the wide range of histology’s explain the high rate of diagnostic discrepancies detected after pathologic revision by expert pathologists.[7] Further on, even if the radiological findings were deceptive in our case reported as chronic granulomatous disease, the decision of the surgeon for the excision biopsy played a major aspect in the treatment of the patient.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Intestinal-type adenocarcinoma of the nasal cavity and paranasal sinuses. Am J Surg Pathol. 1986;10:192-202.
- [CrossRef] [PubMed] [Google Scholar]
- Histologic classification of sinonasal intestinal-type adenocarcinoma. Am J Surg Pathol. 1991;15:368-75.
- [CrossRef] [PubMed] [Google Scholar]
- Primary colonic-type adenocarcinoma of the base of the tongue: A previously unreported phenotype. Hum Pathol. 2009;40:1798-802.
- [CrossRef] [PubMed] [Google Scholar]
- Adenosquamous carcinoma of hypopharynx with intestinal phenotype. Head Neck Pathol. 2015;9:114-8.
- [CrossRef] [PubMed] [Google Scholar]
- Primary pulmonary adenocarcinoma with enteric differentiation. Cancer. 1991;68:1754-7.
- [CrossRef] [Google Scholar]
- Carcinoma of the nasal cavity and accessory sinuses in woodworkers. Lancet. 1967;11:311-2.
- [CrossRef] [Google Scholar]
- Clinical implication of diagnostic and histopathologic discrepancies in sinonasal malignancies. Laryngoscope. 2021;131:E1468-75.
- [CrossRef] [Google Scholar]






