Translate this page into:
A rare cause of abdominal pain: Abdominal epilepsy a diagnosis often missed
-
Received: ,
Accepted: ,
How to cite this article: Bembey RA, Jha RR. A rare cause of abdominal pain: Abdominal epilepsy a diagnosis often missed. Sri Ramachandra J Health Sci 2023;3:33-5.
Abstract
Abdominal epilepsy (AE) is a very rare and easily missed; which is thought to be temporal lobe epilepsy and is usually a diagnosis of exclusion. AE usually affects the pediatric age group. However, there have been recorded occurrences even in adults. AE presents as unexplained, variable severity, relentless, recurrent gastrointestinal symptoms such as paroxysmal pain episodes, nausea, bloating, and diarrhea. These symptoms show significant improvement with antiepileptic therapy. Diagnosis is aided by electroencephalography changes in the temporal lobes associated with symptoms suggestive of central nervous system involvements such as altered consciousness, confusion, or lethargy. Vague nature of the symptoms causes misdiagnosis in most cases, leading to persistent suffering for the patient. We present a case of 35-year-old female who presented with abdominal pain and after extensive workup was diagnosed as a case of AE. She responded well to the treatment and doing well on follow-up.
Keywords
Paroxysmal abdominal pain
Abdominal epilepsy
Somatoform disorder
INTRODUCTION
Nonspecific symptom like abdominal pain can be caused by myriad pathologies, leading to frequent misdiagnosis.[1] Pathological conditions that cause paroxysmal gastrointestinal (GI) symptoms are porphyria, intestinal malrotation, cyclical vomiting, peritoneal bands, abdominal migraine, etc.[2] Many emotional and psychological factors also present as GI symptoms and an accurate diagnosis can be confounded due to these. The accurate diagnosis in such cases is delayed or abandoned due to the attribution of “functional” or “psychogenic” causality, causing the patient to suffer.[3] Physicians usually rule out common causes of pain and if not found, potentially puts patients with rare pain disorders that are a challenge to diagnose, at considerable risk for prolonged suffering. Stigma associated with diagnosis of Somatoform disorder or a medically unexplained symptom is understated.[4] One of the extremely rare cause of abdominal pain is abdominal or autonomic epilepsy.[5] According to International League Against Epilepsy, abdominal epilepsies (AEs) are classified as part of simple or complex partial seizures.[6] This rare epileptic form should be considered in patients with unexplained paroxysmal abdominal pain, migraine-like symptoms, or loss/alteration of consciousness. The diagnosis is confirmed with electroencephalography (EEG) abnormalities showing generalized or temporal epileptiform waveforms along with an exceptional response in symptoms to antiepileptic drugs.
CASE REPORT
A 35-year-old married Indian female, with three children (P3L3A0), presented to our hospital with complaints of recurrent paroxysmal abdominal pain for the past 10 months. It was sudden in onset, colicky in nature, resolving spontaneously and lasting for up to 1 h, and associated with palpitation and stuttering. The attacks occurred at random intervals, with 2–5 episodes/day along with severe nausea, feeling of dizziness, and light-headiness. The pain started in the paraumbilical area and radiated to the lumbar regions. There was no associated vomiting, headache, convulsions, and loss of consciousness but each episode was followed by 2–3 h of somnolence tiredness, lethargy, and increased sleep. The pain was not relieved by oral or injectable pain medications or anti spasmodic administered by local Practitioner. The abdominal pain episodes intensity increased over the last month with few episodes of loss of unconsciousness, which lasted for 10–15 min, with spontaneous recovery of consciousness, not associated with abnormal body movements, uprolling of eyes, tongue biting, post-episode confusion, urinary or stool incontinence, diaphoresis, etc. Her pregnancies were all spontaneously conceived, full-term normal vaginal delivery, and were uneventful with no medical complications. Her vitals were stable except her blood pressure which reduced to around 90/50–80/40 mmHg after every episode of abdominal pain which responded to intravenous (IV) fluid resuscitation. She was a vegetarian with normal bowel bladder and no addictions. On further detailed history, she is a graduate and a housewife by profession told about few episodes of discoloration of urine which after workup was attributed to dehydration. There was so significant past, drug, surgical, or family history. Physical general and systemic examination was all within normal limits. Abdomen was soft and non-tender with normal bowel sounds in between attacks. A gastroenterologist reference was taken. Patient underwent extensive investigation to rule out all differential diagnosis such as celiac sprue, heart arrhythmia conditions, acute intermittent porphyria, inflammatory bowel diseases, abdominal tuberculosis, autoimmune diseases, pancreatitis, heavy metal poisoning, and Wilson’s disease.
Her hemogram, liver function test, kidney function test, urine routine and culture, blood culture, anti-TTg Ab IgA (antibodies to tissue transglutaminase), erythrocyte sedimentation rate, C-reactive protein, antinuclear antibody profile, ultrasound whole abdomen, serum amylase, serum lipase, stool for routine and ova cyst, stool hanging drop and cultures, creatinine phosphokinase (CPK), urine for porphyrin, fecal calprotectin, autoimmune hepatitis panel, serum electrolytes, serum porphobilinogen, serum aminolevulinic acid, serum ceruloplasmin, and serum lead all came out normal and insignificant ruling out celiac disease, porphyria’s, worm infestation, autoimmune diseases, etc. Further upper GI endoscopy and colonoscopy done with biopsy were also normal. A contrast-enhanced computed tomography abdomen was also performed in view of persistent troublesome abdominal pain, but was reported normal. Since no gastrointestinal cause could be found for the abdominal pain, we further did a full cardiology workup to exclude any cardiovascular causes or arrhythmias mimicking the patient symptoms including ECG, transthoracic echocardiography, Trop I, CPK(MB) and 24 hour holter monitoring done which were also normal.
Further, a magnetic resonance imaging brain ordered to rule out neurological problem and was normal. Thereafter, EEG was done which was normal. She was given supportive medication but none helped her abdominal pain episodes. A psychiatrist review taken to rule out psychogenic causes, given mood elevator which did not help. A differential of abdominal migraine was also considered, treated with nonsteroidal anti-inflammatory drugs and triptans but to no avail. On further discussion and repeat detailed history, a continuous EEG recording was done which revealed frequent generalized 4–5Hz spike and wave, polyspike and generalized wave discharges with bifrontal predominance, each discharge corresponding to episode of abdominal pain [Figure 1]. Similar discharges with hyperventilation, photic stimulation and sleep deprivation were recorded, confirming diagnosis of AE.
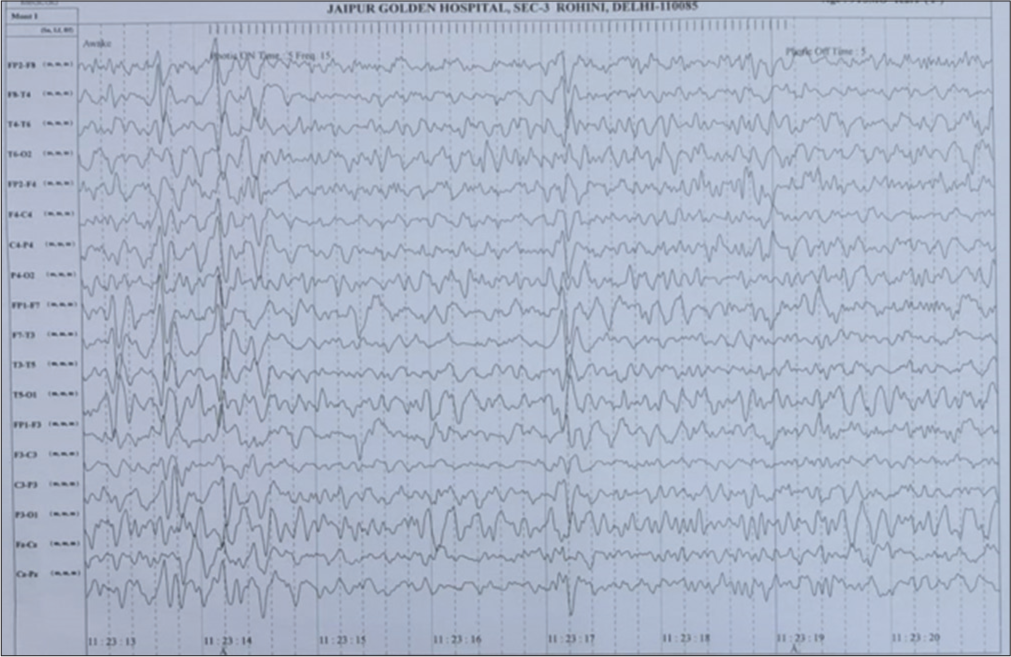
- Electroencephalography taken during abdominal episode showing frequent generalized 4–5Hz spike and wave, polyspike and generalized wave discharges with bifrontal predominance.
Antiepileptics started (Inj. LEVETIRACETAM, 1 g loading dose followed by 500 mg I.V., twice a day). Her abdominal pain episodes responded very well to treatment with significant decrease in frequency and intensity. Her antiepileptic drugs were further titrated up, IV LEVETIRACETAM 500 mg, thrice a day. She was advised regular follow-up and on 1-month follow-up, she had no episode of abdominal pain and repeat EEG was performed and was normal while on antiepileptic treatment. The patient is doing well. Prior informed consent was taken to publish the case taken from patient.
DISCUSSION
To rule out rare causes of abdominal pain like AE, a detailed history and careful clinical examination is a must to evaluate such case. The several “red flag” symptoms and signs include weight loss, unexplained fever, significant vomiting, hematemesis, chronic severe diarrhea, and bleeding per-rectum, which should alert physician about potential diagnosis. First line screening investigations should be done in all cases, which are usually normal like in our case. The main challenge of diagnosis arises after this, to make a proper diagnosis and initiate treatment to prevent prolonged suffering for the patient physically and emotionally. Furthermore, investigative workup is aimed and guided by a revised history and reviewing pain diary made by patient on follow-up. Invasive investigations should be planned as a last resort. Treatment with deworming, laxatives, antibiotics, proton-pump inhibitors, analgesics, and antispasmodics is not helpful in AE. AE frequently presents with GI symptoms such as pain abdomen, nausea, and vomiting, most commonly associated with neurological symptoms include lethargy, confusion, and sleep following or along with a pain episode.
AE is characterized and diagnosed by following diagnostic criteria.[7]
Otherwise unexplained, paroxysmal GI symptoms
Symptoms of central nervous system (CNS) disturbance
EEG is diagnostically abnormal with finding specific for seizure disorder especially if done during episode of abdominal pain
Improvement with anticonvulsant medication.
The pathophysiology of AE is still unknown in this modern era. The gold standard for diagnosis of AE is EEG which shows runs of generalized spikes, high voltage slow waves, and wave discharges or local abnormalities particularly in temporal or frontal lobe. Clinical symptoms show significant improvement along with EEG normalization with levetiracetam, carbamazepine, or oxcarbazepine, as usually the focus for AE lies in temporal lobe, as reported in many studies. Improvement with phenytoin or valproate has also been reported. However, the role of particular antiepileptic drug in AE needs more extensive studies. Recording of normalization of EEG after treatment is a must for diagnosis of AE. AE has many close differential diagnoses such as irritable bowel syndrome and abdominal migraine and needs to be differentiated for timely initiation of treatment. Although the abdominal symptoms of irritable bowel syndrome are similar, it may be distinguished from the AE by the presence of altered consciousness during some of the attacks, a tendency toward tiredness after an attack, and by an abnormal EEG. Difference between AE and migraine is discussed in [Table 1].[8]
| Abdominal epilepsy | Abdominal migraine |
|---|---|
| Pain is of short duration with an abrupt onset | Episodes of pain are wide spread, with inter episode interval ranging from weeks to months. Symptoms should be present for at least 6 months before diagnosis. |
| The pain is usually localized to paraunbilical and epigastric region, rarely spreading to any other body parts | The pain can be diffuse or localized to paraumbilical or midline of abdomen. |
| Episode of abdominal pain is usually followed by post-ictal confusion, excessive sleepiness, dizziness, or lethargy | Patient is asymptomatic post-episode. |
| Not a functional disorder | A functional disorder diagnosed by ROME III H2c criteria |
CONCLUSION
This rare case of AE very distinctively exhibits difficulty in diagnosing the condition and can be time-consuming and challenging as the symptomatology is indistinct. Furthermore, suspicion is low especially in adults, due to less knowledge of AE among physicians. AE is very often overlooked and misdiagnosed and it should be considered as a differential in patients presenting with recurrent, episodic, and paroxysmal GI complaints, but always associated with CNS disturbance which do not respond to standard treatment modalities. After thoroughly reviewing and excluding the more common causes of abdominal pain, AE as a diagnosis should be considered to provide an accurate and timely diagnosis. Physicians should also be aware of the stigma associated with diagnosis of a somatoform disorder in these cases and an affordable and easy to perform test like an EEG, helps furnishing the diagnosis, so that symptoms of such cases are not falsely labeled as “psychogenic” or “functional.” A video EEG is preferable during the abdominal pain episode if available. Once an abnormal EEG is noted, treatment should be initiated on antiepileptic drugs with regular follow-up. Our case report, an uncommon challenging diagnosis of AE was made, wherein the patient improved exponentially with treatment, significantly improving her standard of living.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Long-term follow-up of patients diagnosed with nonspecific abdominal pain (NSAP): Identification of pathology as a possible cause for NSAP. Eur Surg. 2015;47:140-3.
- [CrossRef] [Google Scholar]
- Epilepsy presenting only with severe abdominal pain. J Pediatr Neurosci. 2010;5:169-70.
- [CrossRef] [PubMed] [Google Scholar]
- Chronic abdominal wall pain misdiagnosed as functional abdominal pain. J Am Board Fam Med. 2013;26:738-44.
- [CrossRef] [PubMed] [Google Scholar]
- Coding of medically unexplained symptoms and somatoform disorders by general practitioners-an exploratory focus group study. BMC Fam Pract. 2018;19:129.
- [CrossRef] [PubMed] [Google Scholar]
- Recurrent abdominal pain: When should an epileptic seizure be suspected? Arq Neuropsiquiatr. 2002;60:628-30.
- [CrossRef] [PubMed] [Google Scholar]
- Abdominal epilepsy, an uncommon cause of chronic and recurrent abdominal pain: A case report. Clin Case Rep. 2016;4:1117-9.
- [CrossRef] [PubMed] [Google Scholar]
- Neurologic etiology of episodic abdominal pain: Epilepsy vs. Migraine. IAIM. 2018;5:179-83.
- [Google Scholar]







