Acute exacerbation of chronic suppurative otitis media by Vibrio cholerae O39 – A case report
*Corresponding author: Tessa Antony, Department of Microbiology, Sri Ramachandra Medical College and Research Institute, Chennai, Tamil Nadu, India. drtessa@sriramachandra.edu.in
-
Received: ,
Accepted: ,
How to cite this article: Antony T, Anandan Y, Somu L, Sekar U. Acute exacerbation of chronic suppurative otitis media by Vibrio cholerae O39 – A case report. Sri Ramachandra J Health Sci 2022;2:40-2.
Abstract
Vibrio cholerae is gram-negative bacilli belonging to the Vibrionaceae family generally found in brackish and marine water. Based on the O antigen on the cell wall of the bacteria, they are divided into three major subgroups – V. cholerae O1, V. cholerae O139, and V. cholerae non-O1/non-O139. The serogroups O1 and O139 harboring cholera toxin gene cause diarrhea, while the non-O1/non-O139 can cause a milder diarrhea and extraintestinal infections. We report a case of acute exacerbation of chronic suppurative otitis media by V. cholerae O39, which is classified in the non-O1/non-O139 group. The patient presented with slowly progressive painful ear discharge which evolved over a period of 3 months. V. cholerae O39 was isolated from the ear discharge by culture and confirmed by serologic and molecular testing. The patient improved symptomatically with 1 week of treatment with intravenous ciprofloxacin and tobramycin ear drops.
Keywords
Vibrio cholerae
Otitis media
Ear discharge
INTRODUCTION
Infections of the ear can be broadly divided into those affecting the external ear (otitis externa) and those affecting the middle ear (otitis media). Otitis media can be acute or chronic. Chronic suppurative otitis media is inflammation of the middle ear and mastoid cavity with recurrent ear discharges. The organisms isolated from chronic otitis media include aerobic bacteria – Pseudomonas aeruginosa, Staphylococcus aureus, Proteus spp., and Klebsiella pneumoniae which are common followed by rarer anaerobic bacteria – Bacteroides spp., Clostridium spp., Peptostreptococcus spp., and Prevotella melaninogenica.[1] Vibrio cholerae -non-O1/non-O139 can cause a wide range of extraintestinal manifestations such as wound infections, ear infections, meningitis, septicemia, peritonitis, biliary, and urinary tract infections.[2] This case is reported to increase awareness among clinicians and microbiologists regarding the possibility of V. cholerae being an etiological agent for otitis media and the importance of adequate antibiotic therapy based on antimicrobial susceptibility.
CASE REPORT
An adult male patient in his mid-thirties presented to the otorhinolaryngology department with complaints of discharge from the right ear for 3 months which was insidious in onset and progressive in nature. The discharge was mucopurulent, foul smelling, and not blood stained. It was associated with ear pain. He had found the ear discharge to be aggravated in the preceding 1 month following bath in the sea near Tiruchendur. Tiruchendur is located at the Coromandel Coast off the Bay of Bengal, in the state of Tamil Nadu (India). The patient did not have accompanying fever, giddiness, or tinnitus. His history was unremarkable except for recurrent bilateral otitis media since childhood. Tympanoplasty was performed on the left ear 7 years ago with complete resolution of symptoms in that ear.
Ear swab was taken from the right ear of the patient and sent for culture. Gram stain from the specimen revealed few pus cells and plenty of short slender gram-negative bacilli. Culture was performed on sheep blood agar, chocolate, and MacConkey agar. On sheep blood agar, gray-colored colonies with a wide zone of hemodigestion were observed which became dry and wrinkled after 48 h of incubation at 37°C [Figure 1]. Pale nonlactose-fermenting colonies were observed on MacConkey agar. Darting type of motility was observed by hanging drop method. Subsequently, culture was performed on thiosulfate-citrate-bile salts-sucrose (TCBS) agar which produced moist yellow sucrose-fermenting colonies on overnight incubation [Figure 2]. With conventional biochemical testing, the isolate was identified as V. cholerae [Table 1]. String test was done with 0.5% sodium deoxycholate which was found to be positive. Slide agglutination test was performed for serogrouping with antisera, since the strain was auto agglutinating, the results could not be obtained.
| Laboratory tests | Identification | |
|---|---|---|
| Oxidase Catalase |
Positive | Belongs to Vibrionaceae family |
| Indole | Positive | |
| Triple sugar iron | Acid slant/acid butt and no gas production | |
| Mannitol motility medium | Fermented and motile | |
| Hanging drop | Darting motility | |
| String test (0.5% sodium deoxycholate) positive | V.cholerae | |
| Microscan walkaway 96 plus | V.cholerae | |
| OmpW (outer membrane protein W) based PCR | V.cholerae | |
| Serological analysis | V.cholerae O39 | |

- Wrinkled colonies of Vibrio cholerae O39 on blood agar with a wide zone of hemodigestion after 48 h of incubation at 37°C.
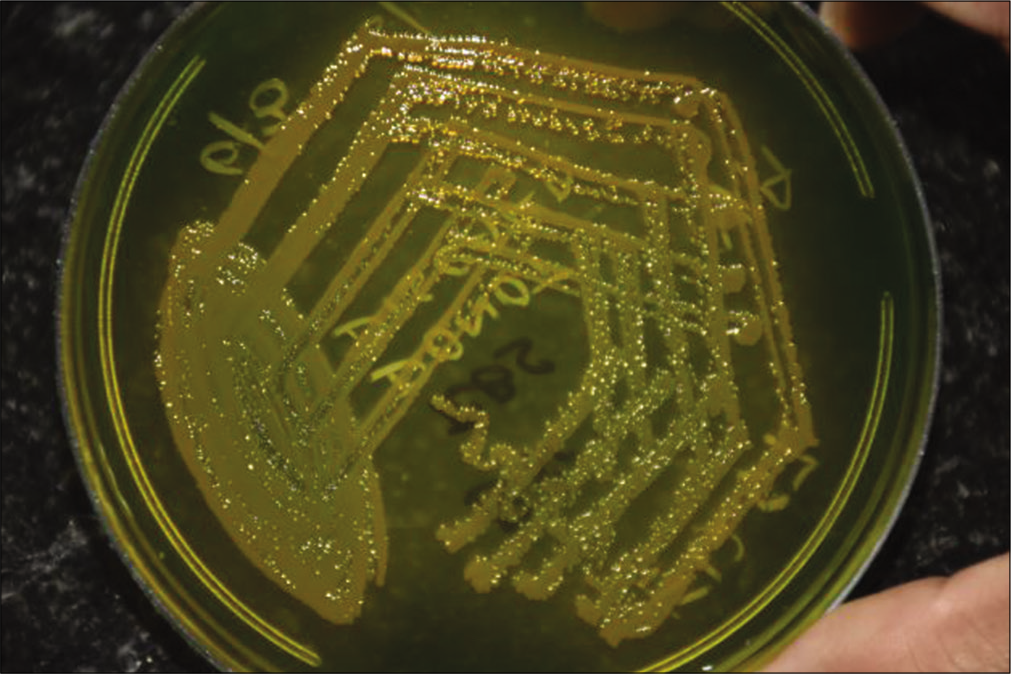
- Yellow colonies of Vibrio cholerae O 39 on TCBS agar after 24 h of incubation at 37°C.
The colonies on MacConkey agar were subjected in a commercial automated identification system – MicroScan WalkAway 96 Plus (Beckman Coulter, United States of America). The organism was identified as V. cholerae with 99.9% probability. It was found to be susceptible to ampicillin, cephalosporins, aminoglycosides, fluoroquinolones, chloramphenicol, tetracycline, and trimethoprimsulfamethoxazole by Kirby–Bauer disk diffusion method on cation adjusted Mueller-Hinton agar. Clinical and Laboratory Standards Institute guidelines (M45, 2018) were used as reference for interpretation of zone size. Further confirmation and serogrouping were done in the National Institute of Cholera and Enteric Diseases (India). OmpW (outer membrane protein W)-based PCR confirmed the isolate to be V. cholerae and another PCR confirmed that the strain did not harbor the ctxA (cholera toxin) gene. Further battery of serological testing revealed the strain to belong to V. cholerae O39. The patient was treated for 1 week with intravenous ciprofloxacin 200 g twice a day and tobramycin ear drops. He improved symptomatically with reduction in ear discharge and pain. A repeat ear swab culture done 2 weeks later did not grow any bacteria.
DISCUSSION
V. cholerae is known to produce cholera toxin and toxincoregulated pilus which are important in causing diarrhea. The other virulence factors which favor colonization and evasion of host defense mechanisms include hemagglutinin, outer membrane proteins, proteases, and type III secretion system.[3] Vibrios produce multiple colony morphologies on non-selective media like blood agar. Some rare V. cholerae isolates produce extremely wrinkled colonies on non-carbohydrate-containing media, which are due to the production of a unique extracellular polysaccharide that confers the property of biofilm formation.[4] This wrinkled morphology was exhibited by the strain isolated from the patient which would have helped in colonization following exposure.
Diarrhea caused by V. cholerae is treated with antibiotics only if the patient is severely ill, has comorbidities, in pregnant women, and those who are severely dehydrated. The antibiotic of choice is doxycycline followed by tetracycline, trimethoprim-sulfamethoxazole, and ciprofloxacin. The extraintestinal infections caused by V. cholerae are treated with antibiotics and are usually found to be susceptible to beta-lactams, fluoroquinolones, tetracycline, trimethoprimsulfamethoxazole, aminoglycosides, and chloramphenicol according to the previous literature.[4] V. cholerae infection of the ear presents as otitis externa or otitis media. A review of the published case reports showed that otitis media by V. cholerae usually follow damage to the ear drum either due to trauma or following recurrent middle ear infection. V. cholerae non-O1/O139 isolates from patients with ear infection were found to be uniformly susceptible to ampicillin, cephalosporin, cotrimoxazole, and fluoroquinolones.[5] The patients were treated with ciprofloxacin ear drops and intravenous third-generation cephalosporins in severe infections and recovered uneventfully following antibiotic therapy.[1,6]
Most of the reports of otitis media by V. cholerae non-O1/non O139 in temperate regions were reported in summer months following exposure to swimming pool, lake, or seawater. The patient had exposure to seawater in December so such variation is not observed in the tropics where it is warm throughout the year. V. cholerae can be identified in the microbiology laboratory by conventional culture and biochemicals. The commercial automated identification systems such as API 20E, Crystal E/NF, MicroScan Neg ID 2, Rapid Neg ID 3, and Vitek can correctly identify only 63%–81% of these organisms to the species level.[7] Therefore, it is important to use conventional biochemical methods for identification to support the automated identification systems. Molecular techniques like polymerase chain reaction (PCR) targeting outer membrane protein W (Omp W) are very useful in rapid identification of V. cholerae isolates.[8] Majority of cases of otitis media or otitis externa caused by V. cholerae non-O1/O139 has been reported from European countries and the United States of America.[1,6] This is the first report of otitis media caused by V. cholerae O39 from India.
CONCLUSION
V. cholerae can be a cause of chronic recurrent otitis media and can remain undiagnosed unless the ear discharge is sampled, sent for culture and appropriate treatment initiated.
V. cholerae can be a cause of otitis media persons who have a breach in the ear drum due to past ear infections and exposed to contaminated seawater.
V. cholerae infections can occur throughout the year in tropics as opposed to the warmer months in temperate region.
Acknowledgment
We would like to thank Dr. Asish Kumar Mukhopadhyay (Scientist F) and his team at National Institute of Cholera and Enteric Diseases, Kolkata, for performing the serological and molecular work to identify the isolate as V. cholerae O39.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Chronic otitis media following infection by non-O1/non-O139 Vibrio cholerae: A case report and review of the literature. Eur J Microbiol Immunol (Bp). 2020;10:186-91.
- [CrossRef] [PubMed] [Google Scholar]
- Extraintestinal infections caused by non-toxigenic Vibrio cholerae non-O1/non-O139. Front Microbiol. 2016;7:144.
- [CrossRef] [PubMed] [Google Scholar]
- Synergistic effect of various virulence factors leading to high toxicity of environmental V. cholerae non-O1/non-O139 isolates lacking ctx gene: Comparative study with clinical strains. PLoS One. 2013;8:e76200.
- [CrossRef] [PubMed] [Google Scholar]
- Vibrio and related organisms In: Carroll KC, Jorgensen JH, Landry ML, Funke G, Warnock DW, eds. Manual of Clinical Microbiology (10th ed). Washington, DC: ASM Press; 2011. p. :666-76.
- [CrossRef] [Google Scholar]
- Occurrence of Vibrio cholerae serogroups other than O1 and O139 in Austria. Wien Klin Wochenschr. 2007;119:235-41.
- [CrossRef] [PubMed] [Google Scholar]
- Otitis media caused by V cholerae O 100. A case report and review of the literature. Front Microbiol. 2017;8:1619.
- [CrossRef] [PubMed] [Google Scholar]
- Accuracy of six commercially available systems for identification of members of the family vibrionaceae. J Clin Microbiol. 2003;41:5654-9.
- [CrossRef] [PubMed] [Google Scholar]
- Rapid method for species-specific identification of Vibrio cholerae using primers targeted to the gene of outer membrane protein OmpW. J Clin Microbiol. 2000;38:4145-51.
- [CrossRef] [PubMed] [Google Scholar]







