Translate this page into:
Juvenile nasopharyngeal angiofibroma tumor – Diagnosis and management in our tertiary hospital
*Corresponding author: Jeric Ashwin Fernando, Department of ENT, Head and Neck Surgery, Sri Ramachndra Institute of Higher Education and Research, Chennai, Tamil Nadu, India. jericash22@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Fernando JA, Saravanam PK, Jayagandhi SK. Juvenile nasopharyngeal angiofibroma tumor – Diagnosis and management in our tertiary hospital. Sri Ramachandra J Health Sci 2022;2:36-9.
Abstract
Juvenile nasopharyngeal angiofibroma (JNA) is a rare benign tumor described by slow progression, vigorous growth, high vascularization, and increased recurrence rate. The aim of this article is to describe a case of JNA from our tertiary hospital and discuss the diagnosis and management in our current practice. A 16-year-old male patient presented with bleeding from the left nasal cavity. On examination, there was a non-pulsatile ovoid like mass occluding the entire left nasal cavity which was able to probe medially, superiorly, and laterally except inferiorly and on probing and it resulted in minimal bleed. Cold spatula test revealed decreased fogging on the left side. Contrast-enhanced computed tomography scan of the paranasal sinuses and nose showed the presence of a large ill-defined heterogeneously enhancing soft-tissue density mass lesion with its epicenter in posterior part of the left nasal cavity and left pterygopalatine fossa and was extending into the left orbit and left cavernous sinus. Complete embolization of the left nasopharyngeal vascular mass was done preoperatively. Two days post-embolization, surgical excision of JNA under general anesthesia was done. The approach was done through sublabial incision. This classic case of JNA was operated endoscopically because of its benefits over the conventional methods.
Keywords
Juvenile nasopharyngeal angiofibroma tumor
Clinical aspects
Diagnosis
Treatment
INTRODUCTION
Hippocrates described juvenile nasopharyngeal angiofibroma (JNA) tumor as a benign lesion with vigorous transformation.[1] It has 0.05-05% incidence of head and neck neoplasms.[1] Young adolescent males between 14 and 25 years are affected.[2] JNA orignates from the superior margin of the sphenopalatine foramen and will eventually invade into the bone, extend into the infratemporal fossa , orbit and middle cranial fossa.[2] Epistaxis, unilateral nasal block, and a nasopharyngeal mass paving the way for the diagnosis of nasopharyngeal angiofibroma.[2,3]
“Diagnosis is obtained by complete general history, clinical/local examination, radiographical examination, and nasal endoscopy and by histopathology if reveals a fibrocellular stroma filled with multiple spindle cells and irregular arrangement of collagen interspersed with an irregular vascular pattern.”[3]
Diagnosis of JNA is done by complete case history, clinical examination, radiographical examination, nasal endoscopy; and specialized imaging techniques such as CT.[4] Due to its high vascularity, angiography is performed to identify the primary vessels and embolization is done to reduce intraoperative blood loss.[3,5]
“Surgical excision is the initial treatment of choice for JNA, especially when intracranial involvement is excluded from the study.” “Traditional open surgical approaches consist of transpalatal, transmaxillary, LeFort 1 osteotomy, and infratemporal fossa craniotomy.”[5,6] Contrastive to open surgery, transnasal endoscopic surgery has less morbidity, better amplifying visualization, lower intraoperative blood loss, and a lower rate of recurrence.[6] Reported recurrence rates vary from approximately 25–55%.[6]
CASE REPORT
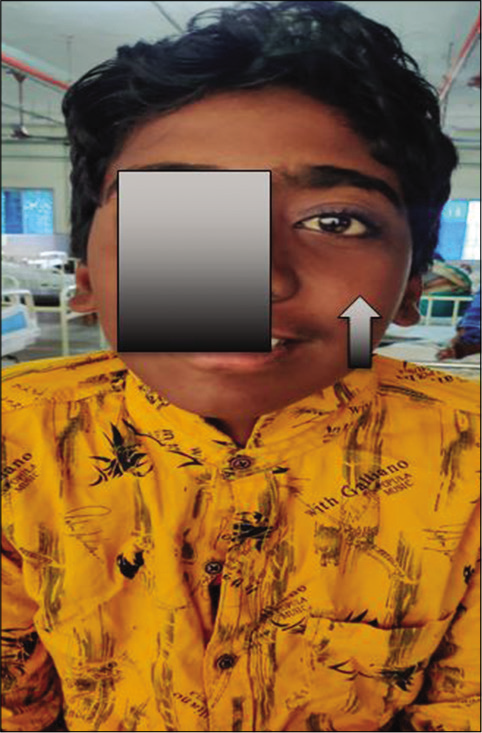
A 16-year-old male patient presented to our OPD with the complaints of multiple episodes of bleeding from the left nasal cavity which was intermittent in nature for a month and lasting for about 10 min (15–20 drops – each episode) which resolved spontaneously. In the last episode of nasal bleed, he had to undergo nasal packing to control epistaxis in an outside hospital for which no records were available. He also gave a history of bilateral nasal blockage and recurrent upper respiratory tract infection for 1 month. There was no significant family history or medical history noted. (Figure 1 showing left eye proptosis for which written consent was taken).

- Pre-operative image (left eye proptosis).
On examination, his vitals were stable. On local examination, there was minimal proptosis of the left eye [Figure 1]. On local examination, there was a non-pulsatile mass occluding the entire left nasal cavity which was able to probe medially, superiorly, and laterally except inferiorly which resulted in minimal bleed. Cold spatula test revealed decreased fogging on the left side. No paranasal sinuses tenderness was elicited. Diagnostic nasal endoscopy showed deviated nasal septum to right, a single pinkish cystic mass with a smooth vascularized, ovoid surface occupying left nasal cavity which bleeds on touch and was hanging which was from middle meatus and occupying the choana. “Contrast-enhanced CT scan of the paranasal sinuses and nose was showed that the presence of a large poorly defined heterogeneously enhancing soft-tissue density mass lesion of size 5.9 × 7.1 × 4.3 cm is noted, with its epicenter in posterior part of the left nasal cavity and left pterygopalatine fossa and was extending into the left orbit and left cavernous sinus; bulging into temporal fossa (extradural); and causing mild indentation of the left temporal lobe” [Figure 2a-c]. It showed erosion of the left pterygoid plates and sphenoid sinus with walls extending into masticator space. It also projects into nasopharynx. Arterial feeders were seen from the left maxillary artery. Mild mucosal thickening was seen in bilateral maxillary, frontal, and left ethmoid sinuses. It also revealed deviation of the nasal septum into the right side which had caused atrophy and compression of the right-sided turbinates. Decision of JNA, soft-tissue tumor, and nasopharyngeal polyp/vascular tumor was made.
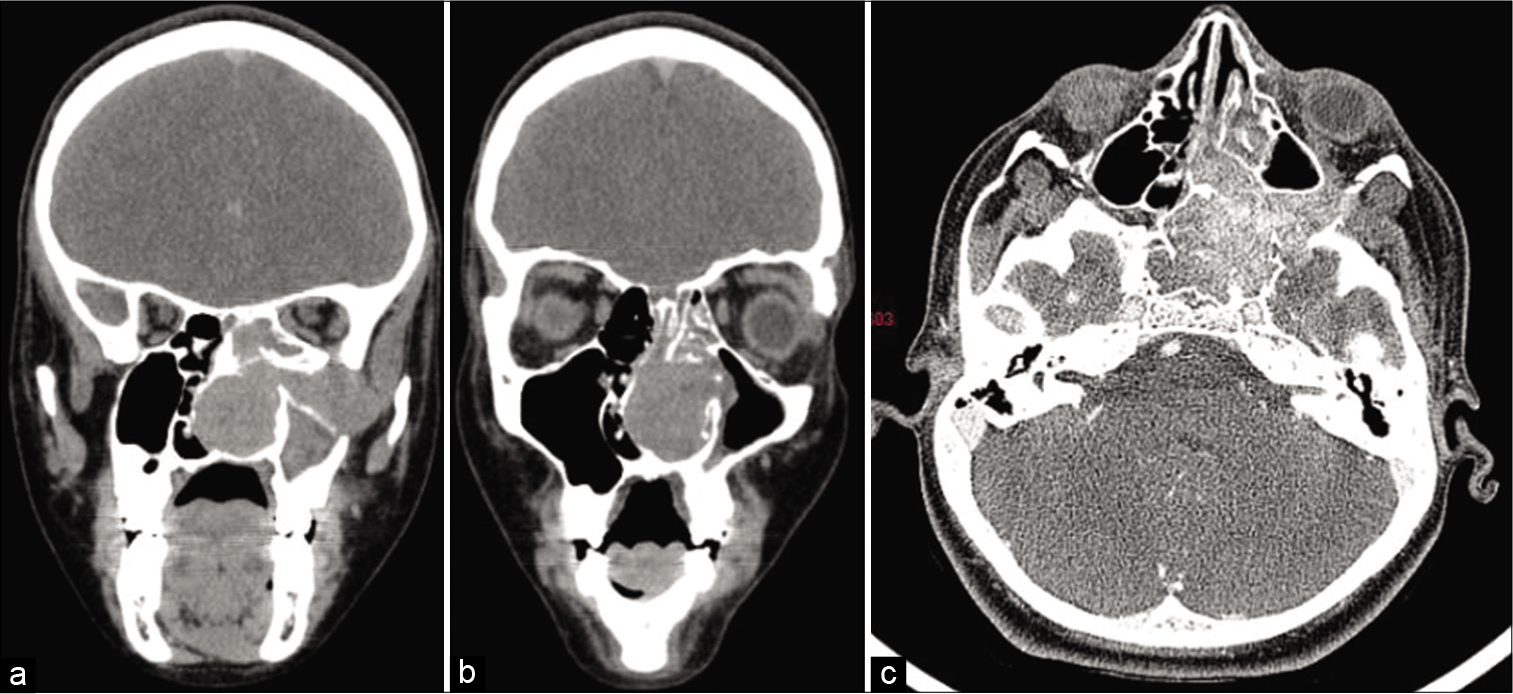
- (a-c) A large ill-defined heterogeneously enhancing soft-tissue density mass lesion of size 5.9 × 7.1 × 4.3 cm is noted, with its epicenter in posterior part of the left nasal cavity and left pterygopalatine fossa and was extending into the left orbit and left cavernous sinus.
Near-complete embolization of the left nasopharyngeal vascular mass under monitored anesthetic care was done preoperatively. An abnormal blush was noted in the left nasopharyngeal and cavernous region with predominant arterial supply from the distal branches of the left internal maxillary, ascending pharyngeal artery and through the dural branches of from the left ICA which was embolized using gelfoam slurry by the interventional radiologists. Two days post-embolization, surgical excision of JNA under general anesthesia was done. The approach was through sublabial incision. Under 0 degree endoscopic vision, the mass was seen filling the pterygopalatine fossa extending into the infra temporal fossa laterally, into the sphenoid sinus in midline pushing the septum to right [Figure 3a and b]. The entire tumor was removed in toto using endoscope and sent for histopathological examination [Figure 4]. Histopathology report showed features consistent with JNA and microscopy findings showed fragments of tissue with abundant blood vessels of varying size and caliber lined by single layers of endothelial cells with a background of plump fibroblasts [Figure 5]. Post-operative period was uneventful [Figure 6].
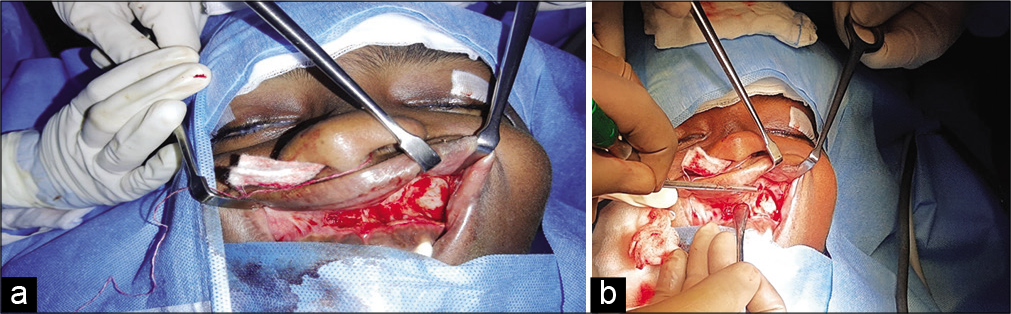
- (a and b) Intraoperative image showing sublabial incision.
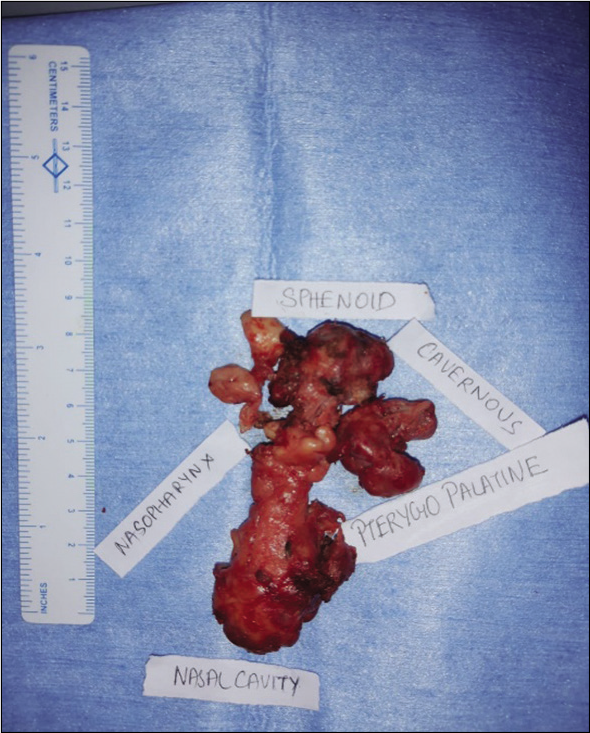
- Surgical removal of juvenile nasopharyngeal angiofibroma – specimen.
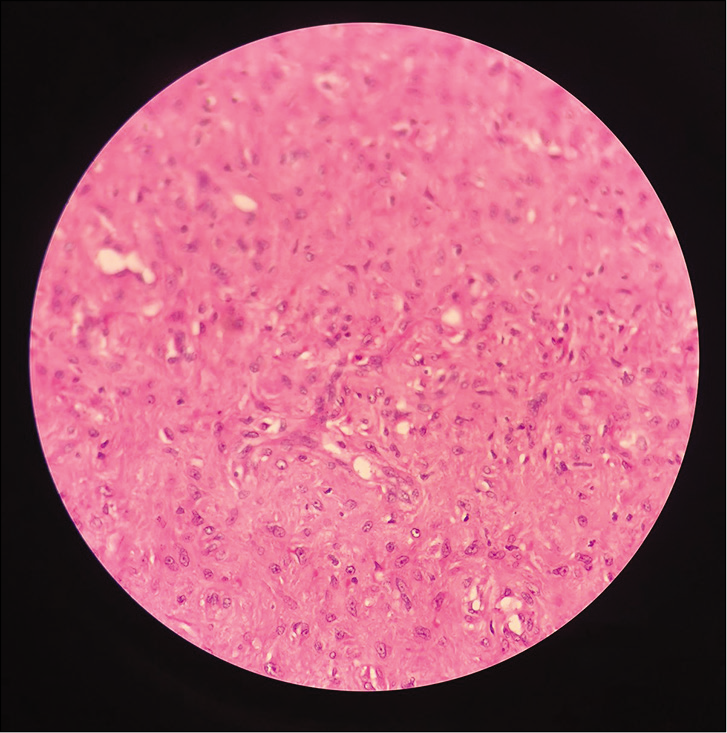
- Histopathological image.
- Post-operative image.
DISCUSSION
JNA between tumor presenting mostly in adolescent males presenting at the age of 14 years. Exclusivity in males is hypothesized as androgen dependence of the tumor.[7] JNA is benign but locally destructive. Due to this invasion and extension, they have high recurrence rates of 0–57%.[7] It has a tendency to grow agree through bones, instead of only occupying space. Etiopathogenesis of angiofibromas can be either developmental, hormonal, or genetic.
“Chandler et al. proposed several staging systems for JNA.”[7] This has been majorly accepted to determine the tumor site and extent. Fisch classification is currently used widely.[7]
In this case, CT scan showed the presence of a large ill-defined heterogeneously enhancing soft-tissue density mass-like lesion extending into the left orbit and left cavernous sinus. Similar findings were reported in other JNA case reports.[8] Anteriors feeders were seen from the left maxillary artery. Similar findings were found in a bilateral JNA case report.[6]
Pre-operative embolization has been shown to reduce perioperative blood loss and is now considered standard preparation for surgery.[9] Similarly, in our case, pre-operative near-complete embolization of the left nasopharyngeal vascular mass lesion was done using gelfoam slurry under monitored anesthesia care 2 days before the surgery.
There are various treatments suggested for JNA, but, lately, the interest in endoscopic resection has increased.[10] Our case followed an open surgical procedure after the embolization as the size of the tumor was large.
“Early investigation and treatment are essential for a good survival rate in JNA. Differential diagnosis includes antrochoanal polyp, rhinosporidiosis, malignancynasopharyngeal carcinoma, lymphoma, rhabdomyosarcoma, nasopharyngeal cyst, and pyogenic granuloma.”[10] Advanced lesions with orbital and intracranial extension have a high recurrence rate. When diagnosed early, the patients are treated with a combination of pre-operative embolization and surgical resection which provide good prognosis.[9,10] Radiotherapy must be reserved for inoperable cases. “Recurrence rates depend on the clinical staging of tumor.”[10]
CONCLUSION
We reported this case to suggest an approach to a JNA case both before and after operation. We wanted to emphasize that angiofibroma can be treated using the endoscopic approach because of its superiority over the traditional methods. We also aimed to warn physicians about a nasal mass when presented a punch biopsy may cause extensive bleeding.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Juvenile Nasopharyngeal angiofibroma: Imaging Characteristics and pre-operative embolization. Bahrain Med Bull. 2016;38:230-2.
- [CrossRef] [Google Scholar]
- Juvenile Nasopharyngeal Angiofibroma: Case report with review on role of imaging in diagnosis. Contemp Clin Dent. 2015;6:98-102.
- [CrossRef] [PubMed] [Google Scholar]
- Juvenile nasopharyngeal angiofibroma. J Oral Maxillofac Pathol. 2016;20:330.
- [CrossRef] [PubMed] [Google Scholar]
- Genetic alterations in juvenile nasopharyngeal angiofibromas. Head Neck. 2008;30:390-400.
- [CrossRef] [PubMed] [Google Scholar]
- Imaging in the diagnosis of juvenile nasopharyngeal angiofibroma. J Clin Imaging Sci. 2013;3(Suppl):1.
- [CrossRef] [PubMed] [Google Scholar]
- Angiofibroma: Changes in staging and treatment. Arch Otolaryngol Head Neck Surg. 1996;122:122-9.
- [CrossRef] [PubMed] [Google Scholar]
- Nasopharyngeal angiofibromas: Staging and management. Ann Otol Rhinol Laryngol. 1984;93:322-9.
- [CrossRef] [PubMed] [Google Scholar]
- Extended osteoplastic maxillotomy for total excision of giant multicompartmental juvenile nasopharyngeal angiofibroma. Indian J Dent Res. 2008;19:366-9.
- [CrossRef] [PubMed] [Google Scholar]
- Preoperative angiography and external carotid artery embolization of juvenile nasopharyngeal angiofibromas in a tertiary referral paediatric centre. Clin Radiol. 2013;68:1097-106.
- [CrossRef] [PubMed] [Google Scholar]
- Exclusive endoscopic resection of juvenile nasopharyngeal angiofibroma: A systematic review of the literature. Otolaryngol Head Neck Surg. 2014;150:350-8.
- [CrossRef] [PubMed] [Google Scholar]






